Complex skin tissue grown in lab from iPSCs
Scientists from Japanese institutions including the RIKEN Center for Developmental Biology and Tokyo University of Science have successfully grown and transplanted into mice complex lab-grown skin — complete with hair follicles and sebaceous glands — from iPSCs.
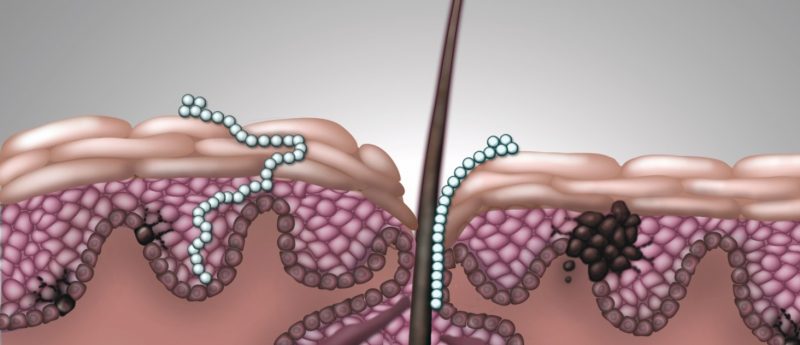
Most patients requiring functioning skin transplants such as burn victims currently receive grafts from a donor site elsewhere on their body, which results in another area of skin that needs healing and is not feasible in patients with full-body burns. Epithelial cells have previously been successfully grown into implantable ‘skin’ sheets, but they have not included the oil-secreting and sweat glands required for fully functioning skin tissue.
A team of scientists, including from the RIKEN Center for Developmental Biology (CDB) and Tokyo University of Science (both Japan), have successfully developed complex, 3D skin tissue in the laboratory from reprogrammed iPSCs. The tissue has hair follicles and sebaceous glands, and formed proper connections with other organ systems such as nerves and muscle fibers when transplanted into mice.
“Up until now, artificial skin development has been hampered by the fact that the skin lacked the important organs, such as hair follicles and exocrine glands, which allow the skin to play its important role in regulation,” explained Takashi Tsuji of the RIKEN Center for Developmental Biology. “With this new technique, we have successfully grown skin that replicates the function of normal tissue. We are coming ever closer to the dream of being able to recreate actual organs in the lab for transplantation, and also believe that tissue grown through this method could be used as an alternative to animal testing of chemicals.”
The team extracted gum cells from the mice and reprogrammed them into iPSCs using reprogramming factors then an embryoid body using Wnt10b. Next, they implanted the embryonic body cells into immune-deficient mice, where they differentiated as for an actual embryo. The cells were then transplanted them out of the nude mice and into the skin tissue of other mice, where they developed normally as integumentary tissue and made normal connections with the surrounding nerve and muscle tissues.
Although the researchers state this success will take 5—10 years to translate into humans, it has brought bioengineered skin replacement therapy one step closer to being a reality. Furthermore, the method could also be adapted to manufacture realistic skin samples for animal-free drug or cosmetic testing.
John McGrath, a professor of molecular dermatology at King’s College London (UK), believes this study was a substantial step forward: “[Today’s skin grafts] function, but they don’t really look like or behave like skin. If you don’t have the hair follicles and you don’t have the sweat glands and things, it’s not going to function as skin…There will be lots of benefits for immediate use, as well as for translational science.”
Sources: Takagi R, Ishimaru J, Sugawara A et al. Bioengineering a 3D integumentary organ system from iPS cells using an in vivo transplantation model. Sci. Adv. 2(4), e1500887 (2016); http://www.bbc.co.uk/news/science-environment-35946611#?utm_source=twitterfeed&utm_medium=twitter; http://www.riken.jp/en/pr/press/2016/20160402_1/