Study uncovers master regulator able to induce maturation of functional insulin-producing cells
Researchers from the Salk institute have successfully generated therapeutically functional glucose-responsive beta that are able to rescue diabetes in type 1 diabetic mice
Scientists from the Salk Institute (CA, USA) have elucidated a longstanding problem in the effort to create replacement cells for diabetic patients. For the first time, the team uncovered a master regulator that, when flipped, induces pancreatic cells to respond to glucose. The result is the production of hundreds of millions of lab-produced human beta cells which are able to rescue diabetes in mice. The findings were recently published in Cell Metabolism.
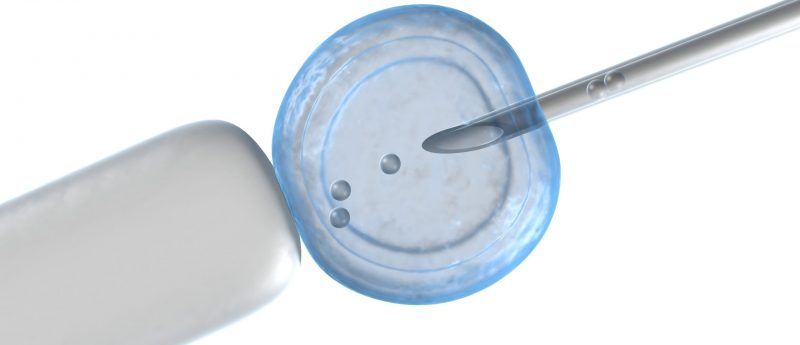
For more than a decade, scientists have been working towards replacing failing pancreatic beta cells linked to immune destruction in children (type 1 diabetes) or obesity-associated diabetes in adults (type 2 diabetes). Although cells made in vitro were able to produce insulin, they were inactive or simply unable to respond to glucose.
“We found the missing energy switch needed to produce robust and functional human beta cells, potentially turning this discovery into a viable treatment for human diabetes,” explained Ronald Evans, co-senior author and director of the Gene Expression Laboratory at Salk. The team began by reprogramming induced pluripotent stem cells into insulin producing, yet not functional, pre-beta cells.
“Pancreatic beta cells must be able to do two things to work effectively: respond to glucose and produce insulin,” commented Evans. “No one had been able to figure out how to make pancreatic cells from human patients that can do both until now.”
The Salk team uncovered numerous molecular switches in beta cells, called transcription factors, that were switched off but had the potential to regulate the transition to a fully functional state. The Salk team discovered a protein switch, called ERR-gamma, which they found was crucial to awaken dormant beta-like cells that were now able respond to glucose and release insulin accordingly.
“This advance will result in a better controlled insulin response than currently available treatments,” observed Michael Downes, co-senior author and a Salk senior staff scientist. “Previously there was nothing known about the maturation process in beta cells. We peeked into that black box and now we know what’s going on.” The team’s technique is an easy, fast and inexpensive way to produce transplantable human pancreatic beta cells in a dish that genetically match patients, added Downes.
“When we added ERR-gamma to pre-diabetic beta cells in a dish, we successfully created a glucose-responsive, beta-like cell,” stated Eiji Yoshihara, first author of the paper and a Salk research associate. “And when we remove ERR-gamma from animals, the glucose response is eliminated, proving that the factor is the master regulator of maturation for the beta cell.”
The Salk researchers discovered that when the matured beta cells were transplanted into type 1 diabetic mice, the procedure quickly rescued their diabetes. “Hopefully, this mirrors what would happen in the clinic–after someone is diagnosed with diabetes they could potentially get this treatment,” concluded Evans. “It’s exciting because it suggests that cells in a dish are ready to go.”
The Salk team is now hoping to take the research to human trials within the next few years.
Sources:
Eiji Yoshihara, Zong Wei, Chun Shi Lin et al. ERRγ Is Required for the Metabolic Maturation of Therapeutically Functional Glucose-Responsive β Cells. Cell Metabolism, doi: http://dx.doi.org/10.1016/j.cmet.2016.03.005 (2016) [Online before print]; www.salk.edu/news-release/salk-scientists-find-secret-sauce-for-personalized-functional-insulin-producing-cells/