Could new gene therapy be the solution to pulmonary edema?
A team of researchers discovered that a new AAV-based gene therapy reduces vascular leakage and may hold potential as a pulmonary edema treatment.
Following a collaborative project between Boston Children’s Hospital (BCH) and Wyss Institute for Biologically Inspired Engineering at Harvard University (both MA, USA), a team of researchers have discovered a potential target for gene therapy that would allow the treatment of pulmonary edema with minimal side effects.
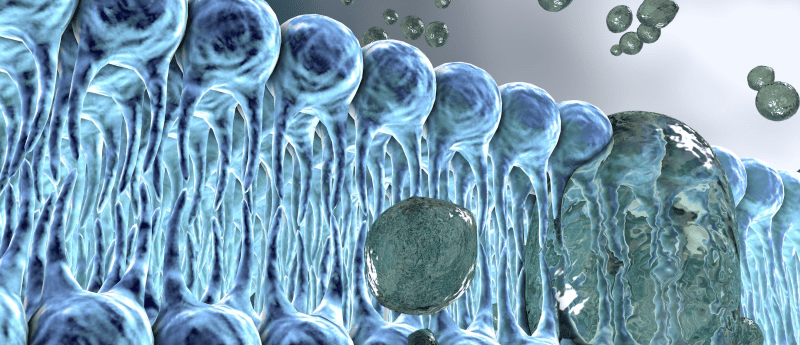
Pulmonary edema occurs in approximately 80% of individuals with heart failure and can prevent patients from being able to do everyday activities due to liquid leaking into their lungs and reducing the amount of oxygen absorbed. Unfortunately, there is currently no treatment available to directly treat the leakage.
This advance in research, published in APL Bioengineering, involved a new adeno-associated virus (AAV)-based gene therapy that could overexpress the HH domain of the CD98hc protein, as well as studies utilizing primary human lung cells in their clinically relevant model, Lung Alveolus Chip.
“Pulmonary edema is similar to a leak in a water pipe. The most effective thing to do is to plug the leak, but current drugs on the market work to shut off the water supply altogether and hope the leak fixes by itself,” commented co-author Ratnakar Potla (Wyss Institute for Biologically Inspired Engineering). “With our method, we can actually target the leak, which is a much more efficient way to address the problem.”
During their investigation, the team focused on the TRPV4 channel protein, which is located in the membrane of lung cells and regulates the flow of substances between the lung’s alveoli and blood vessels. When TRPV4 is put under physical strain it is activated, causing lung tissue to become more ‘leaky’ and resulting in more pressure being put on the surrounding blood vessels. This creates a dangerous feedback loop that progressively worsens pulmonary edema.
Currently, there are drugs in clinical trial developed to chemically shutdown TRVP4; however, the channel plays an essential role in many other processes, such as bone remodeling and bladder tone. Therefore, the inactivation of TRVP4 can cause undesirable side effects that would limit the amount of drug that could be delivered.
Instead, the team of researchers decided to shift their focus onto a different membrane protein, CD98hc, which is responsible for transmitting mechanical forces to TRPV4 and has previously been shown to be able to prevent its mechanical activation. The team hypothesized that a gene therapy delivering a specific region of CD98hc could be an effective treatment for vascular leakage that leads to pulmonary edema.
Following this hypothesis, AAVs were utilized to overexpress the highly homologous (HH) domain of the CD98hc protein, resulting in the cells that overexpressed the HH domain displaying an almost complete inhibition of mechanically-activated calcium-signaling via TRPV4. Furthermore, drugs could still be used to stimulate TRPV4 chemically and restore the calcium signaling response, demonstrating that gene therapy is able to leave the rest of the channel’s functionality intact.
The researchers then investigated the effect of the HH domains overexpression in a human ‘Lung Alveolus Chip’, which has previously been developed at the Wyss Institute as a clinically relevant model of the human lung. They discovered that when their gene therapy vector was introduced, leakage was greatly reduced, plus the barrier strength of the lung cells remained intact, even when under physical strain.
“Remarkably, we saw a significant improvement in lung function even though only about 30% of the lung epithelial cells and 10% of the vascular endothelial cells were successfully transduced with the gene coding for the HH domain of CD98, indicating that this strategy is extremely protective,” commented co-author Rachelle Prantil-Baun (Wyss Institute for Biologically Inspired Engineering).
The researchers analyzed the cells in the Lung Alveolus Chip using fluorescence imaging in order to determine how blocking mechanical activation was providing this protection. They discovered that without gene-therapy the liquid in the air channel was able to lead to breaks in the cell—cell junctions that help maintain the integrity of the air-liquid barrier.
Further, they also observed a difference in the behavior of endothelial cells. Usually these cells rearrange so they are perpendicular to the direction of force being applied, however, those with the AAV gene delivered did not. This resulted in the population of cells being more stable and preserving the cell—cell junctions.
Going forward, the authors hope that the findings from this study can lead to the development of specific mechanotherapeutic drugs for more targeted treatment of pulmonary edema.
Sources: Li J, Wen AM, Potla R et al. AAV-mediated gene therapy targeting TRPV4 mechanotransduction for inhibition of pulmonary vascular leakage. APL Bioeng. doi: 10.1063/1.5122967 (2019) (Epub ahead of print); https://wyss.harvard.edu/news/a-lifeline-for-leaky-lung-cells/
Have any additional questions about this story? Ask us in the comments, below.
Find out more in these top picks from the Editor:
- Study discovers placental stem cells that can repair the heart after heart attack
- Novel regeneration method to repair severely damaged lungs
- Regenerating thyroid and lung function through differentiated iPSCs: an interview with Darrell Kotton