Injectable hydrogel enables controlled release of oxygen to repair post-heart attack cardiac tissue

In this article, Geoffrey Potjewyd (University of Manchester, UK) reviews a recent report from Scientific Reports.
Geoffrey Potjewyd1
1Regenerative Medicine & Neuroscience PhD student, University of Manchester (UK)
During a heart attack, cardiac tissue is starved of oxygen, causing potentially fatal cardiac cell damage. Recovery and protection of cardiac tissue from further damage is crucial. One current therapeutic option is through oxygen supplementation, which increases oxygen levels in the blood and can subsequently improve cardiac function. There have been multiple different animal and clinical studies which have had mixed results. The one common feature of the oxygen based animal and clinical trials is that the route of administration is systemic, and the treatment is very acute lacking a long-lasting oxygen administration.
A group from The Ohio State University (USA) are using a regenerative medicine approach to post-heart attack oxygen delivery, using drug-releasing (oxygen in this case) hydrogels. These hydrogels are loaded with oxygen and injected directly to the site of cardiac injury. The physical properties of the hydrogel allow for a controlled release of oxygen, thereby increasing the therapeutic window of the oxygen administration.
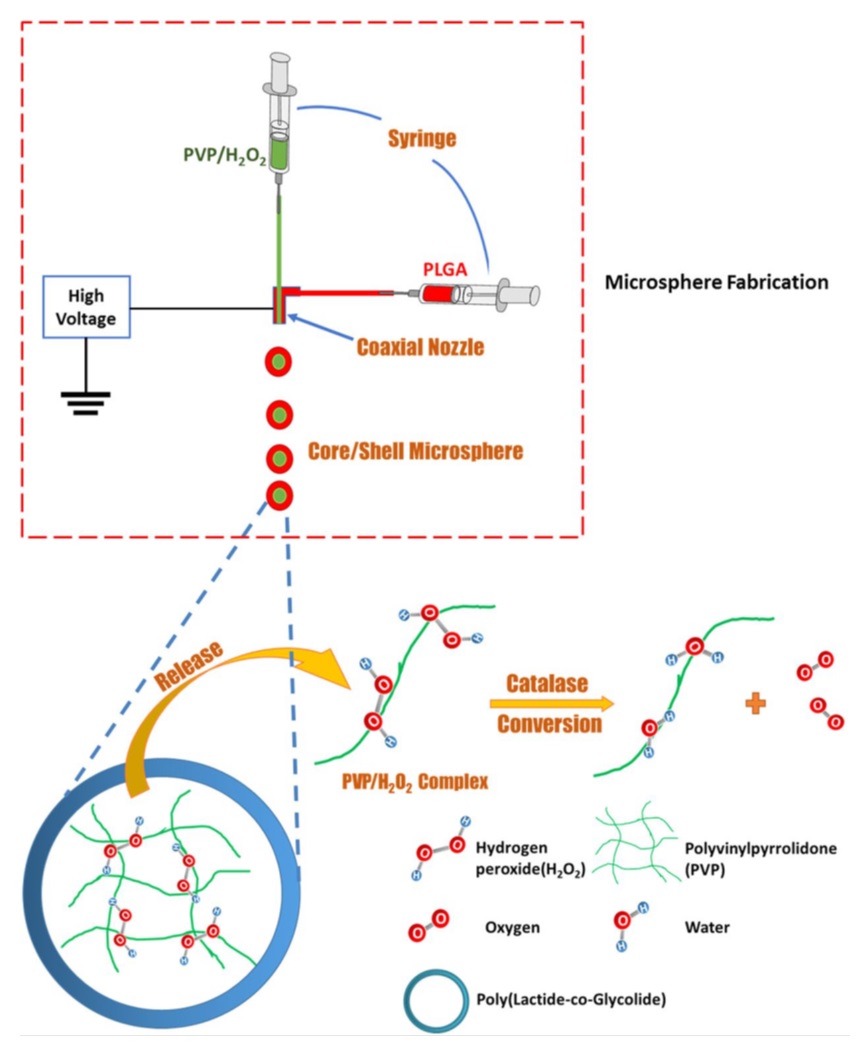
The hydrogel system is composed of oxygen containing microshperes (PVP/H202) encapsulated around an injectable hydrogel polymer shell (PLGA) (Figure 1). This construct is created through a biofabrication technique similar to 3D printing, called electrospraying. As hydrogen peroxide (H202) is broken down to oxygen and released from the hydrogel it is able to elicit an effect on surrounding tissue.
The oxygen releasing hydrogel was tested with both cardiac cells in vitro, and in a rat model following a surgically induced heart attack.
The group established that the hydrogel based oxygen release system could deliver oxygen over a 4-week period, with oxygen levels peaking at 24.8% after 7 days and decreasing to 11.2% at the end of the 4 weeks. This controlled oxygen release resulted in a significant improvement in cardiac function; with reduced cardiac fibrosis, increased cardiac cell survival, promoted angiogenesis, and reduced infiltration of immune cells.
To evaluate the effects of the oxygen release-system in vitro, a 3D collagen hydrogel was used to model native tissue. This collagen hydrogel was seeded with cardiac cells to assess the cellular and molecular output when the oxygen release system is injected into the hydrogel and without this injection.
The use of an in vitro model allowed for precise control over conditions, whereas an inherent issue of creating ischemic events like heart attacks or strokes in animal models is that the amount of damage performed is inevitably variable in different animals. The group was able to compare the effects of the oxygen-release system in precise hypoxic conditions (1% O2), establishing that cardiac cell survival was greatly increased at this level of oxygen deprivation as well as reducing myofibroblast formation. The reduction in myofibroblast formation is crucial to avoiding scarring which is common and damaging after heart attacks.
This system offers an alternative therapeutic option following a heart attack, with current medicating regimes involving blood thinning drugs like aspirin and warfarin, which can lead to further complications. Additionally, this system may be used to aid recovery after open heart surgery, potentially speeding up the damage caused by both the initial heart attack and the reparative surgery.
This system also has a potential role in other disease treatments, with conditions like stroke and vascular dementia potentially benefiting from a controlled oxygen release system. A stroke is effectively a “brain attack”, where a blockage or damage to the blood vessels leading to the brain can cause a severe ischemic event. This damage can reduce the blood flow and oxygen delivery to the brain in recovery, but this injectable oxygen release system may reduce the post-stroke damage which occurs as well as aiding the recovery of the damaged areas.
Zhaobo Fan, Zhaobin Xu, Hong Niu et al. An Injectable Oxygen Release System to Augment Cell Survival and Promote Cardiac Repair Following Myocardial Infarction. Sci. Rep. 8, 1371 (2018)