Overcoming challenges in laryngeal and tracheal restoration: an interview with David Lott, Mayo Clinic
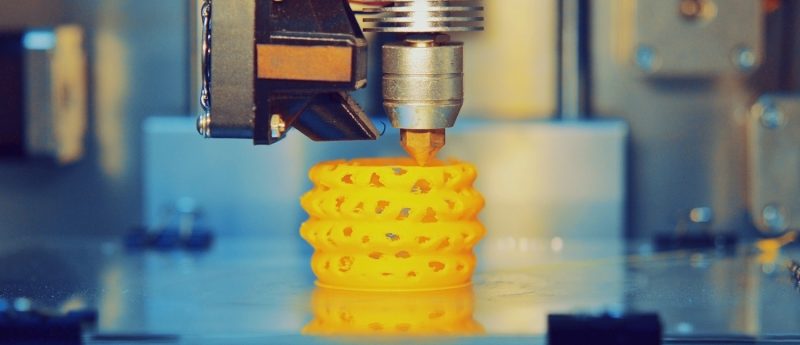
In this interview, David Lott (Mayo Clinic) discusses how 3D bioprinting could enable better post-surgery reconstruction.
Please introduce yourself and your home institution
My name is David Lott, MD. I’m a laryngeal surgeon at Mayo Clinic Arizona, Associate Director, Center for Regenerative Medicine and Director, Mayo Clinic Head and Neck Regeneration Lab.
What are the challenges with human laryngeal transplantation?
The primary challenges lie with the immunosuppression needed for transplantation. The side effects from immunosuppression can be very severe and even life-threatening. Immunosuppression cannot be used in patients with a recent cancer and the vast majority of patients that need a laryngeal transplant are due to cancer. Therefore, most patients in need of a transplant are not able to receive one because of the immunosuppression.
How could 3D printing overcome these?
3D bioprinting uses scaffold materials that the body accepts without needing immunosuppression. In addition, these scaffolds are often seeded with the patient’s own stem cells. Because the cells are from the patient, no immunosuppression is needed. This now provides an option for the vast majority of patients that need laryngeal reconstruction but are not able to have immunosuppression.
What features of laryngeal and tracheal tissue will be the hardest to recreate?
The ciliated lining of the respiratory epithelium is very difficult to recreate. Also, the neural input for the mobile vocal fold joint is difficult to regenerate.
Do 3D printed scaffolds have any advantages over decellularized natural scaffolds?
The main advantage over decellularrized natural scaffolds is the patient’s specificity. A 3D printed scaffold can be created to exactly match the individual patient’s need. In addition, the process of creating the scaffold is much faster and cheaper. The primary disadvantage is that 3D printing cannot exactly replicate the native microstructure of the scaffold.
How are you using this technology?
My lab has developed a 3D printed hemilarynx (half larynx) for reconstruction of defects from cancer excision. Most patients who get a total laryngotomy (total removal of the voice box, usually done to treat cancer) don’t need to have the entire larynx removed due to the cancer involving the entire larynx.
The total laryngectomy is usually done because we can’t fix the defect (hole) that is left behind and the patient wouldn’t have a functional voice box — meaning they can’t speak, swallow, or breathe without a trach tube. This implant allows us to reconstruct the defect at the time of surgery and prevents the patient from having the entire larynx removed. Additionally, no immunosuppression is needed.
We are using 3D printed scaffolds in larynx reconstruction now! The addition of stem cells will need to wait a while longer while we work with the FDA. Our hope is that we can soon share this technology with other facilities to help even more patients. In addition, this foundational platform allows for expansion of this technology to other areas of the body.
What does the future hold for bioengineered tissue for human transplantation?
The future is very exciting. In the not too distant future, an entire larynx may be 3D printed with vibrational vocal folds and mobility of the joint. This will prevent thousands of patients from needing a laryngectomy.