3D printing in radiation oncology: where are we now?

In this interview, James Robar (Dalhousie University; NS, Canada) discusses the current landscape of 3D printing in radiation oncology and explains how collaboration in this space is driving innovation.
Biography
 James Robar PhD, FCCPM
James Robar PhD, FCCPM
Chief of Medical Physics at the Nova Scotia Health Authority; Professor of Radiation Oncology at Dalhousie University ( both NS, Canada)
James Robar PhD, FCCPM is the Chief of Medical Physics at the Nova Scotia Health Authority and Professor of Radiation Oncology at Dalhousie University, both in Halifax (NS, Canada). Dr. Robar divides his time between clinical practice and research, with interests in image guidance technology in radiation oncology, dose enhancement using gold nanoparticles and novel applications of 3D printing technologies. Dr. Robar is the author of over 30 scientific articles and holds multiple licensed patents related to advancing state-of-the art radiation therapy techniques. He is a co-founder and board member of Adaptiiv Medical Technologies Inc. (Adaptiiv; NS, Canada), which has produced the world’s first FDA-approved software solution employing 3D printing intended for use in the radiation oncology sector. Dr. Robar completed his Doctorate in Medical Physics at the University of British Columbia (Vancouver; BC, Canada), his clinical residency in oncology physics at the BC Cancer Agency (BC, Canada). He is a Fellow of the Canadian College of Physicists in Medicine and has been practicing in Nova Scotia since 2003.
Could you briefly describe your role and how your work involves 3D printing in the medical space?
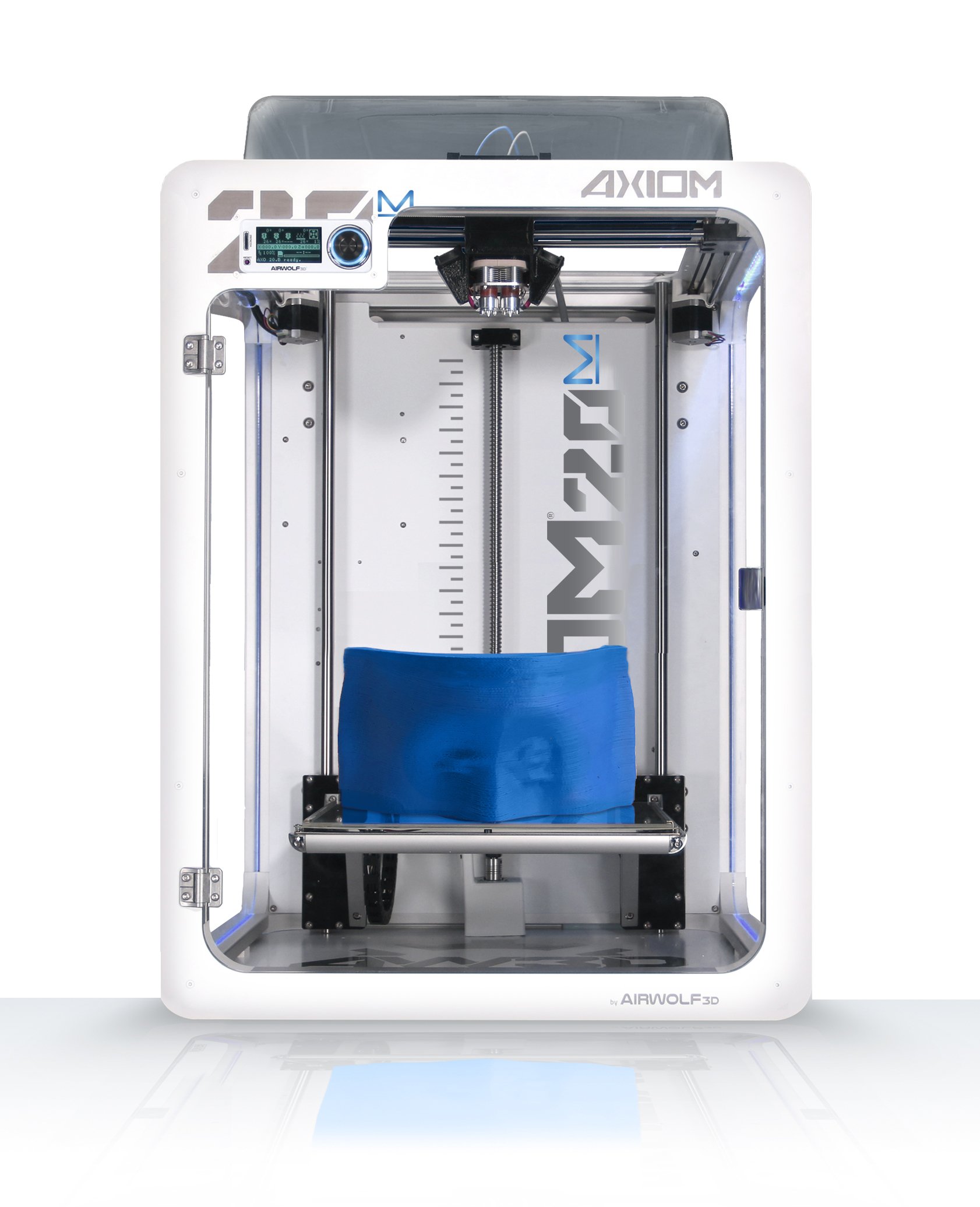
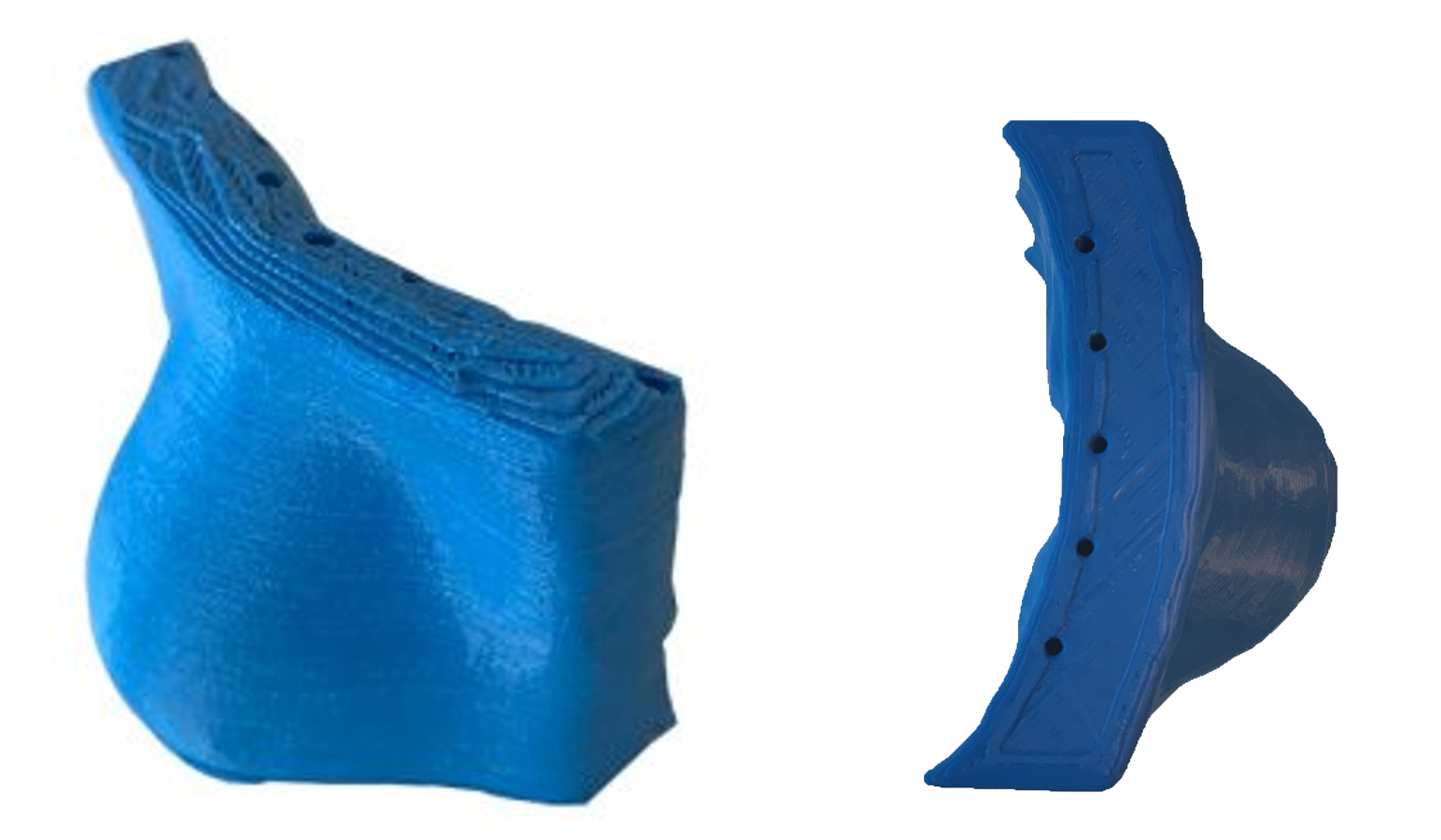
I am a medical physicist specializing in the area of radiation therapy (RT), which is a non-invasive treatment used for over 50% of all cancer patients in the management of their disease. Various RT techniques require generation of a patient-specific, physical accessory that must be fabricated to match the particular anatomy of the patient. For example, a bolus is an approximately tissue-equivalent layer of material that is fitted to the skin surface of the patient when treating superficial tumors. The purpose of the bolus is to allow the radiation dose to build up to a sufficient level at the location of the tumor. Accuracy in producing this accessory is key, since inadvertent air gaps can cause errors in radiation dose delivery. Prior to the development of 3D printing clinical solutions, these accessories were either generic and often ill-fitting — or were produced through painstakingly manual methods, e.g., crafting of wax or molded thermoplastics, processes that were limited with regard to accuracy, error-prone, resource-intensive and expensive. Over the past 3 years, our team at Dalhousie University has licensed applicable IP to Adaptiiv and has collaborated closely with their team to supplant manual methods with more accurate, versatile and efficient 3D printing solutions.
What first attracted you to the idea of adopting 3D printing technologies? What are the key challenges 3D printing has helped you to overcome?
Radiation oncology is a dynamic profession that uses among the most sophisticated treatment delivery technologies in medicine. For example, external beam radiation therapy is administered using a clinical linear accelerator (linac), an approximately US$2.5M machine that accelerates electrons close to the speed of light, then produces shaped, high-energy x-ray beams that kill cancer cells with millimeter precision. In another approach, High Dose Rate (HDR) surface brachytherapy, a machine called an afterloader precisely inserts a radioactive source at pre-defined locations and durations within the patient’s tumor to develop a radiation dose distribution from the inside-out. Both technologies are powered by sophisticated treatment planning software (TPS) applications, allowing accurate prediction of radiation dose distributions in three dimensions based on the individual patient’s 3D CT and MRI imaging.
Until several years ago, these impressive technologies were often combined with conspicuously low-tech, manual methods of patient setup and application of accessories. This was not only discordant with the rest of the technology suite but could also be disconcerting to patients.
When 3D printing became widely accessible circa 2012, my research team set out to make manually fabricated accessories, such as bolus and generic brachytherapy applicators, obsolete.
In this context, the allure of 3D printing was threefold: improved accuracy, increased efficiency and a more comfortable and reassuring experience for the patient.

What challenges currently exist with regulating 3D-printed solutions within radiation oncology, and do you have any advice to overcome these challenges?
For good reason, software solutions that we employ in RT for planning and delivery require regulatory clearance and the software used to design and produce 3D patient accessories in RT is no exception. This includes, for example, CE Mark clearance in Europe, and FDA 510(k) approval in the USA. Although the regulatory process can be time- and resource-consuming for a small company that is eager to innovate, the regulatory steps are both mandatory and valuable in our field. The alternative, for example, of a medical physicist using non-medical, generic CAD or mesh-handling software to design patient devices involves many irrelevant variables, requires skills and training that practitioners generally do not possess, and has not been rigorously evaluated in the context of RT applications.
In developing its first products, the approach that Adaptiiv adopted was pragmatic: from a materials point of view, the regulatory requirements for 3D-printed devices simply placed on the skin were less demanding than, e.g., devices placed in cavities inside the body. Thus, photon and modulated electron bolus solutions were not only in demand but were natural as first choices. Even so, regulatory requirements necessitated a comprehensive quality management program and thousands of person-hours to identify and test software and printing solutions that would meet the safety and reliability requirements of the RT clinic. Now that clearance has been issued for photon bolus, electron bolus and surface brachytherapy applicators, Adaptiiv is building upon this experience and portfolio toward clearance of intracavitary brachytherapy applicators and other devices in the RT domain, partnering with international thought-leaders in the sector.
What limitations still exist with 3D printing and what would you like to see addressed in order to overcome them?
Speed of both FDM and SLA 3D printing remains a limitation, although in most cases 3D printing is still far more efficient than manual fabrication of complex devices. One can expect to spend 1—12 hours printing a typical RT device, depending on the volume. Fortunately, this time is offset by the fact that multiple devices can be printed in a single batch if required and that the printing process requires no user-interaction, so the operational costs remain minimal. In addition, for most of our applications, spatial resolution of printing is not a stringent requirement compared to many other 3D printing tasks, so large-diameter FDM extruders and larger layer heights are often preferred. This offers efficiency advantages: for example, using a 1.2 mm diameter nozzle instead of a 0.5 mm diameter nozzle can reduce print times by a factor of three.
Efficient 3D printing is especially vital in the context of producing ‘adaptive’ patient accessories. It is well known that patient anatomy may change over the course of a multi-day fractionated treatment regimen due to weight loss, tumor regression or edema. Fortunately, our linac platforms can acquire daily 3D cone-beam CT images of the patient and these image data can be used to produce 3D-printed devices that keep pace with the dynamic anatomy. For this application 3D printing methods must be capable of producing new devices quickly, for example, within hours. Even more demanding will be use-cases in intraoperative radiation therapy, where 3D-printed guides or spacers could be invaluable. This would require production of accurate devices within minutes.
Finally, for a host of RT applications it would be useful to offer the option of printing devices that contain high-density metals, for example, in order to incorporate radiation shielding within near tissue-equivalent patient devices. Although metal-infused FDM filaments exist, these do not offer a sufficient density to shield megavoltage photons or electrons. While true metal printing is possible, the current technology needs to become simpler and more cost-efficient for the average clinic. Adaptiiv is innovating in this direction and future solutions will be forthcoming.
What would you say is fueling the uptake of 3D printing technologies within the medical space? How would you say collaboration is driving innovation?
In our experience, additive manufacturing is the technique of choice in two scenarios:
- where bespoke fabrication is needed, often as a one-off device or
- where other manufacturing techniques are simply incapable, labor-intensive, or cost-prohibitive.
Over a gamut of applications in medicine, usually one and often both scenarios apply. An example in our specialization where both criteria apply is the 3D-printed brachytherapy applicator: the device is entirely patient-specific and must contain complex tunnels within the volume of the device. Certainly, production of this device would not be achievable with other methods, especially as an in-house tool in the hands of the practitioner.
Adaptiiv, collaborates with leading research facilities throughout the world to improve our current offerings and develop new, innovative treatment approaches in radiation therapy. These partners of ours have first-hand involvement in the development, design and testing of new products and features. In conjunction with our collaboration partners, we currently have as many as five new modules being developed in our product pipeline.

What will cancer therapies of the future look like if 3D printing technologies continue to benefit approaches to different radiation therapy strategies?
The future is now and 3D printing software/hardware solutions align completely with the broad transition toward individualized patient care in medicine. Several years ago, publications on 3D printing applications in RT focused on basic questions such as radiological properties of materials and achievable accuracy of printing methods. Now there is an emerging body of literature showing positive clinical results for treatment of skin cancers, breast cancer and intracavitary and interstitial brachytherapy indications. Many reports demonstrate an increase of both accuracy, efficiency and in several studies, a reduction of cost and burden on the healthcare system.
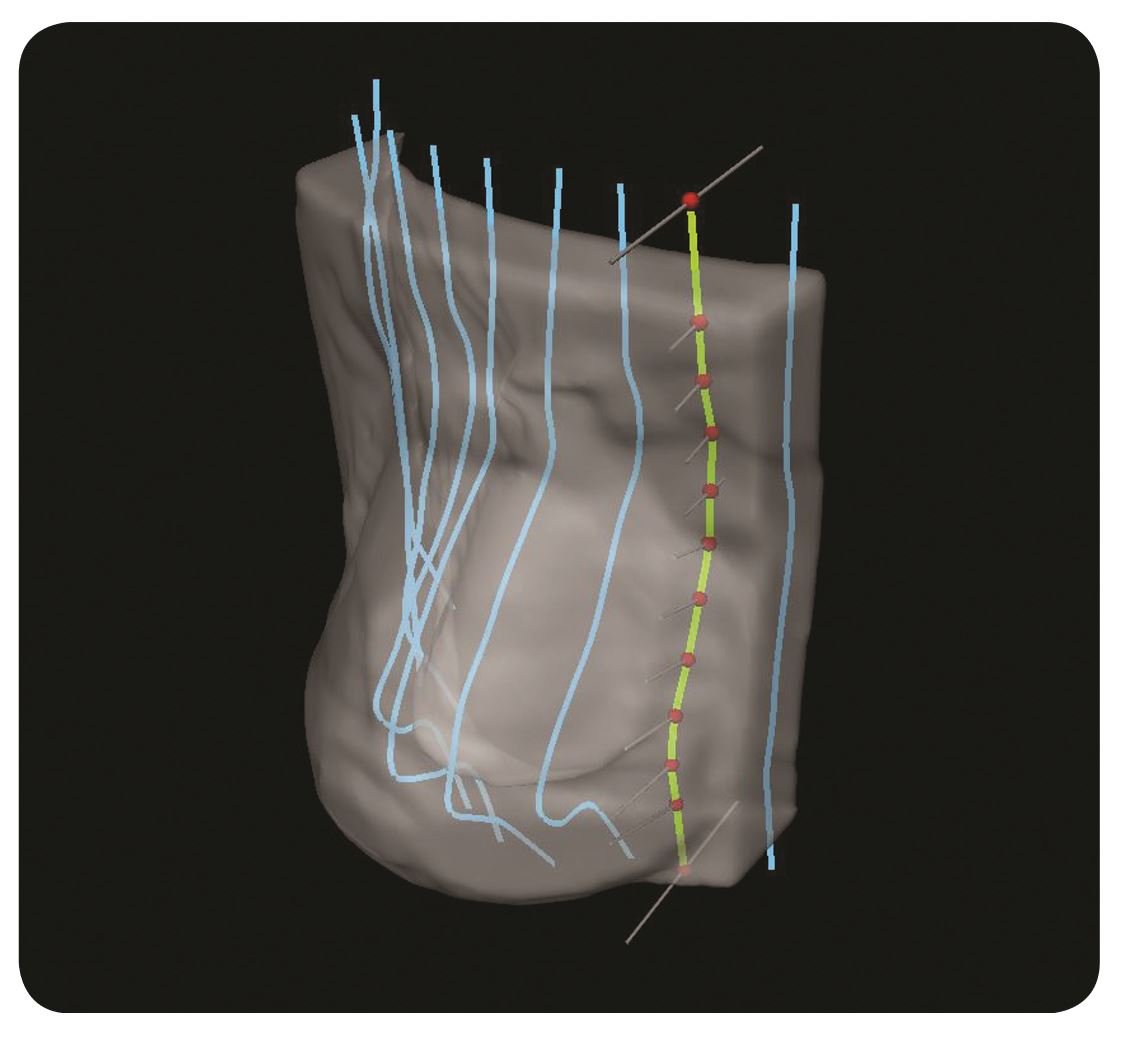
Exciting developments are on the horizon, with expansion of the role of 3D printing in brachytherapy, for example. This will include patient-conforming, interstitial applicators that guide needles precisely according to a predetermined treatment plan. Treatment plan-specific 3D-printed templates are also possible that are used to position needles or applicators. These solutions will require additional R&D, however, and will demand dedicated materials with appropriate biocompatibility characteristics and the capacity for high-temperature steam sterilization between daily treatment fractions. Candidate media exist already and therefore I anticipate that effective clinical adoption of this technology will hinge largely on effective software solutions that integrate smoothly with treatment planning.
Finally, I think we will see interesting developments around 3D printing enabling in vivo dosimetry, which is the measurement of radiation dose delivered to the patient, either during or just after treatment delivery. Adaptiiv, for example, has developed clever software tools for in-printing pockets that house small dosimeters such as Optically Stimulated Luminescent Dosimeters (OSLDs). However, future innovations may involve 3D printing of radiation-sensitive materials, such that the patient device becomes the in vivo measurement tool. This may be an interesting subject for a future 3DMedNet article (stay tuned!).

Since your previous editorial for 3DMedNet (published in June 2016), how has 3D printing progressed as a technology for radiation therapy? Where are we now?
Over the past 3 years in our field, 3D printing has moved from an exploratory endeavor in RT to one that is central to clinical workflow, using dedicated software tools. While early efforts employed general-purpose CAD, mesh-handling or slicer software applications for object design, these tools did not provide a streamlined process. Many clinics are now taking advantage of RT-specific software applications that reduce the time required at the design step from many hours to just a few minutes. In addition to making the process efficient, deployment of a dedicated software application may be required because regulatory-cleared software must be used unless otherwise approved within a research protocol.
3D printing unseats longstanding manual methods, and this transition may take time. But already many clinics are now closing their ‘mould rooms’ — valuable real estate that historically housed plaster of Paris, wax and moldable thermoplastics; these resources are being replaced tidily by one or two compact 3D printers driven by intelligent software solutions. Whereas mould room radiation therapists used to iteratively sculpt in wax, they are now in charge of 3D printing technology and are well positioned to facilitate this transition. Previous trial-and-error processes have become systematic, software-driven and thus provide more uniform results for the patient. 3D printers themselves have become more dependable and at least for our applications, have become much faster over recent years.
Finally, I think we will see the development of 3D printing media that are designed accordingly to meet the specific needs of the RT field. For example, an unfortunate but necessary step in many external beam RT treatments is immobilization of the patient using a rigid mask. The status-quo workflow involves heating up a thermoplastic mesh in a hot water bath until it is soft, then forming the hot and wet mesh around, for example, the head and neck of the patient. Practitioners know that although patients tolerate this process it can be extremely unpleasant and claustrophobia-inducing. Adaptiiv is collaborating with immobilization-system manufacturers toward replacing this process with an automated printing process that can be completed in an automated fashion, even without the patient present. In addition, Adaptiiv is busy engineering specific low-density but rigid media that should serve to minimize the toxicity that is caused by inadvertent build-up by standard mask materials. Thus, the process becomes more efficient, more patient friendly and may help alleviate acute toxicities of the treatment.
This post has been sponsored by: