Alleviating chronic back pain: an interview with Isaac Erickson
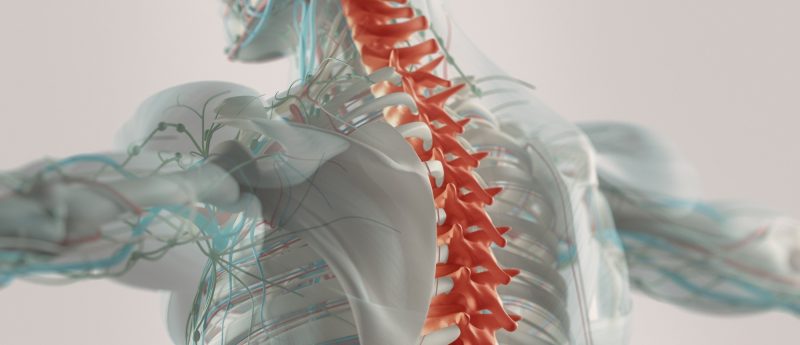
Isaac Erickson, DiscGenics (UT, USA), discusses their allogeneic cell therapy for degenerative disc disease at Phacilitate Leader’s World and World Stem Cell Summit 2020 (FL, USA), as well as scaling up and dealing with different regulatory markets. Can you please introduce yourself and tell us a little about your current role? My name is Isaac Erickson. I've been at DiscGenics (UT, USA) for about four and a half years now. DiscGenics is focused on developing a cell therapy for lower back pain and my role is Director of Bioprocess Engineering. I work mainly on assessing and selecting technologies to enable...