Breaking new ground on an allogeneic immunotherapy
Researchers at the University of California, Los Angeles (UCLA; CA, USA) have produced safe and effective allogeneic immune cells that one day may be mobilized to combat cancer.
Allogeneic cell therapies differ from autologous cell therapies as they utilize cells derived from a healthy donor, as opposed to patient-derived cells that have been engineered to confer therapeutic effects.
Autologous cell therapies are attractive for the treatment of many diseases because of their immunocompatibility and efficacy. However, given their highly personalized nature, manufacturing has significant time constraints. This can impose a serious risk for patients with cancer, who often have time pressure to begin treatment.
The production of effective cancer treatments, like chimeric antigen receptor T cell therapy (CAR-T), from allogeneic sources could alleviate this restriction and thereby improve patient accessibility to potentially life-saving treatment.
CAR-T cell therapies face several challenges in the treatment of cancerous solid tumors, including infiltration barriers, antigen heterogeneity and immunosuppressive tumor microenvironments. In addition to this, they can also have adverse effects, like cytokine release syndrome or graft-versus-host disease (GvHD), which need to be prevented when designing CAR-T therapies.
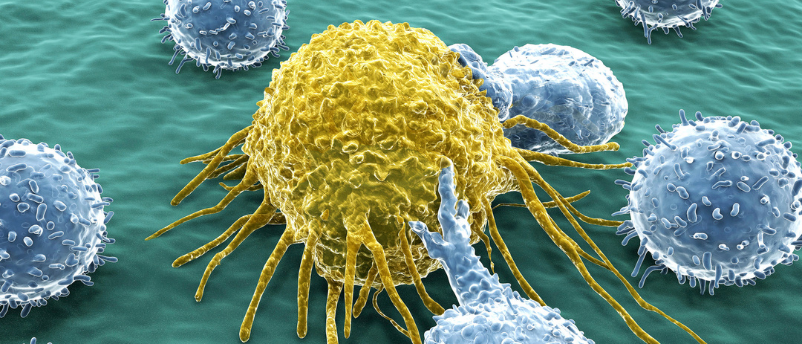
The present study, led by Lili Yang at UCLA, intended to build the foundations for an allogeneic CAR-T cell therapy that was not only capable of overcoming these limitations but did not provoke an immune response. Gamma delta (γδ) T cells formed the focus, as they can target a wide range of cancers without inducing GvHD.
The team screened donor peripheral blood mononuclear cells for high expression levels of a particular biomarker, CD16, which is associated with cell-mediated cytotoxicity. The researchers predicted these to be more potent against cancer cells. This prediction was supported through the elevated expression profiles of genes that encode transcription factors, activation markers and molecules associated with anti-tumor activity.
These screened cells were then engineered to have enhanced anti-tumor activity by introducing chimeric antigen receptors that target mesothelin, a cell-surface glycoprotein that is overexpressed in solid tumour cancers. They were also engineered to have increased interleukin-15 expression, which has been shown to increase persistence of immune and immune-like cells in the body.
These enhanced γδ T cells were tested in vitro on ovarian cancer cell lines. They could attack both the cancer cells and tumor-associated macrophages, which are immune cells that promote cancer growth and potentiate immunosuppression. In addition, in vivo testing using xenografted tumor models demonstrated tumor retardation without GvHD or other adverse health consequences.
“The results of this research shed light on the promising feasibility, therapeutic potential, and remarkable safety profile of these engineered CD16-high gamma delta T cells,” commented Lili Yang, lead author of the study. “We hope this can be a viable therapeutic option for cancer treatment in the future.”
You might also like:
 Oncovirus boosts efficacy of CAR-T cell therapy
Oncovirus boosts efficacy of CAR-T cell therapy
Mayo Clinic (MN, USA) researchers have combined CAR-T cell therapy with an oncolytic virus to produce a new immunotherapy that is more effective at targeting and treating solid tumors than the administration of either treatment alone.