Discovering the mechanisms behind wound healing: an interview with Vicki P Losick
In this interview, Vicki P Losick, PhD, of the MDI Biological Laboratory (Bar Harbor, ME, USA), discusses her research into the pathways involved in wound healing and the considerations involved in translating this knowledge into clinical outcomes.
Wound healing is the dynamic, multi-stage process by which skin and other body tissues repair themselves in the case of disease, trauma or even aging, which can be considered a series of mini-wounds. Effective treatment options are needed to avoid symptoms including pain, odour and risk of infection and to quickly get patients back on their feet.
In a recently published study, Dr Vicki P Losick of the MDI Biological Laboratory (Bar Harbor, ME, USA) discovered a new healing mechanism that she calls wound-induced polyploidy (WIP). The traditional view holds that the size and function of injured or diseased tissue are restored through cell proliferation, but Losick has discovered that WIP accomplishes this through the enlargement of existing cells.
In this interview, she discusses her research into the pathways involved in wound healing and the considerations involved in translating this knowledge into clinical outcomes.

Vicki P Losick, PhD
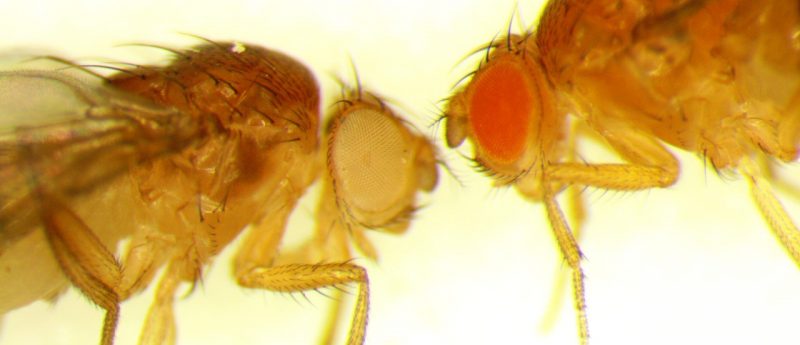
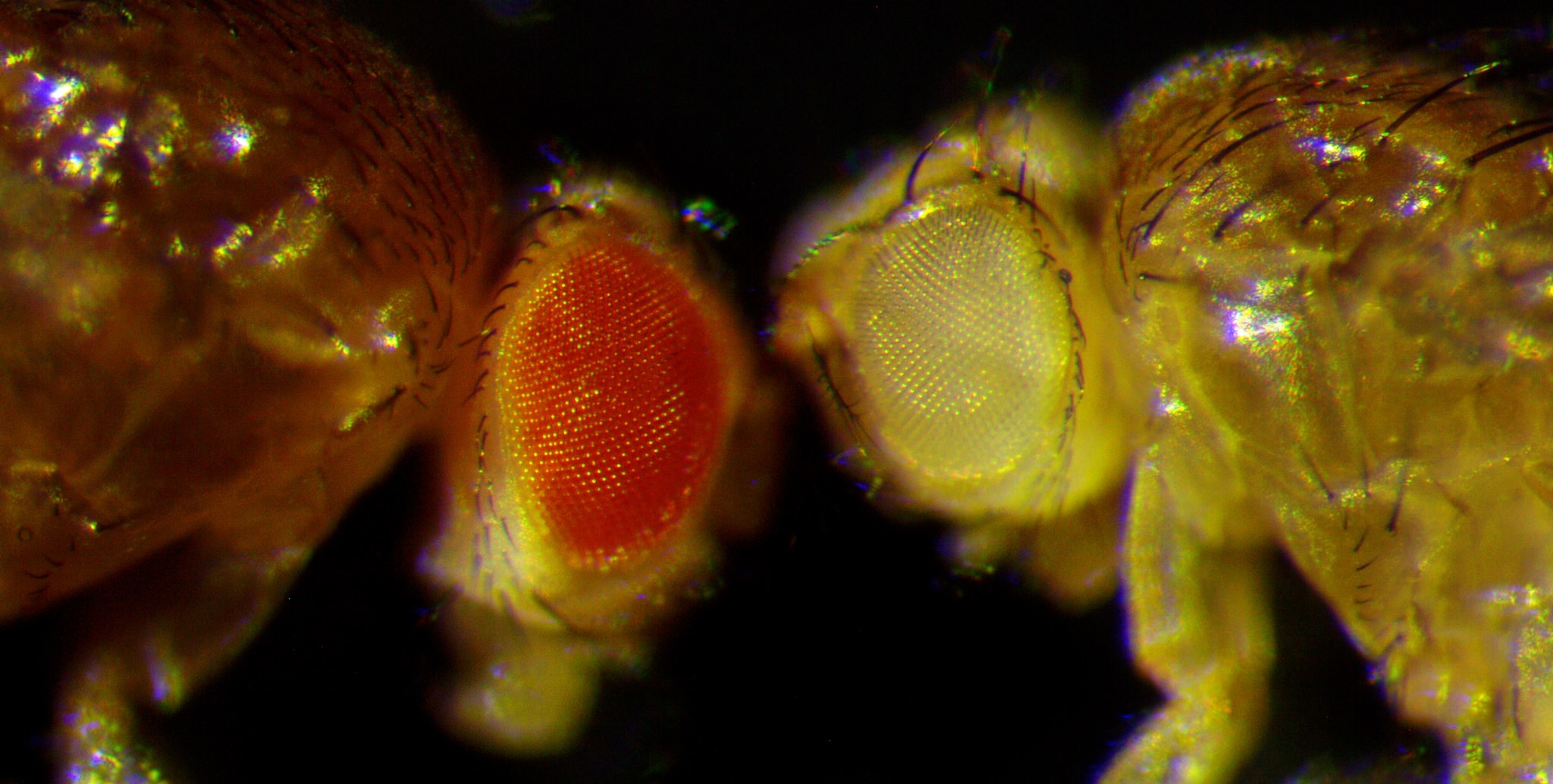
Wound healing typically relies on cell division to replace cells lost to injury, disease or aging, but Dr Losick has found that cells can also be replaced by the creation of extra-large polyploid cells, or cells with more than the diploid number of chromosomes. Wound-induced polyploidy (WIP) appears to be widely used in fruit flies and mice. Dr Losick originally discovered WIP in fruit flies and then found in collaborative work that WIP is conserved and functions in the mouse cornea. She is now studying why WIP occurs and the molecular mechanisms that regulate it with the ultimate goal of improving wound healing in humans.
Can you tell us about yourself and your career to date?
My pursuit of a science career was inspired by a curiosity in the way things work and a desire to tackle problems that I’ve had since an early age. I earned a bachelor’s degree from Bates College (Lewiston, ME, USA) in biochemistry and a PhD from Tufts University School of Medicine (Boston, MA, USA), where I studied how the Legionella pneumophila bacterium causes Legionnaire’s disease.
In my post-doctoral studies I moved beyond microbiology, working with Dr Allan Spradling at the Carnegie Institution for Science (Baltimore, MD, USA) to study how tissues repair themselves in fruit flies. The fruit fly is a great genetic model system that has already yielded significant insights into wound healing, including how embryonic wounds heal and how stem cells maintain identity and function. I wanted to learn more about how adult tissues heal themselves, particularly those that lack a proliferative cell source.
“One of the challenges in the wound healing field is that even though we understand the core steps involved in healing, we still don’t have a good understanding of how different tissues respond to damage.”
What are the biggest challenges in wound healing and why do we need to understand the process better?
One of the challenges in the wound healing field is that even though we understand the core steps (wound healing occurs through a cascade, or sequence, of events in which an inflammatory response occurs, cells are lost and replaced, and either regeneration or remodeling take place), we still don’t have a good understanding of how different tissues respond to damage.
Some tissues, such as skin, have a robust ability to heal, in part because skin contains resident stem cells. For reasons we don’t fully understand, other tissues — heart, for instance — do not have stem cells and as a consequence do not heal as well. We still don’t understand why tissues have different capacities for healing and what mechanisms compensate for cell loss, especially in tissues that don’t regenerate.
Cellular hypertrophy in response to injury has been known for some time. Were you surprised to discover that this is actually a wound healing mechanism?
Yes. I started my postdoctoral research by investigating how tissues made up non-dividing cells undergo repair. At that time, there were many unanswered questions, including ‘Do non-dividing, differentiated cells re-enter the cell cycle and proliferate when injured?’ and ‘How does repair occur?’. To answer such fundamental questions, I created an injury model in the epithelium of the adult fruit fly, which like many tissues in our bodies is made up of differentiated cells that do not divide.
“I was surprised to find that cellular hypertrophy in the fruit fly was actually a critical part of the normal wound healing response. That led me to re-examine all of the examples in our body in which we see cells growing rather than dividing, like the heart, and to reconsider cell growth as part of the organ’s innate ability to repair tissue damage.”
I found that when the adult fruit fly is injured, the injury causes cells to re-enter the cell cycle but, rather than completing mitosis (cell division) the cells around the wound site grow in size by forming giant polyploid cells. This is similar to the cellular hypertrophy response that is seen in the injured adult heart. Heart cells, or cardiomyocytes, have been observed to increase in size and sometimes ploidy in response to injury. I was surprised to find that cellular hypertrophy in the fruit fly was actually a critical part of the normal wound healing response. That led me to re-examine the examples in our bodies in which we see cells growing rather than dividing and to reconsider cell growth as part of the organ’s innate ability to repair tissue damage, instead of as a marker of pathology.
You explained that the cells’ increase in size is due to polyploidization. Are there any risks associated with having cells with extra DNA?
Polyploidization in humans is still poorly understood. Gametes (egg and sperm) are haploid and the rest of our adult cells are either diploid (two sets of chromosomes) or polyploid (more than two sets of chromosomes). Polyploidy is actually more common than many realize. Polyploid cells are required for the development and function of many of our tissues and organs, including the placenta, heart, liver, blood and muscle. Giant trophoblast cells, which make up the placenta, have 256 pairs of chromosomes. These extra-large cells are required for the placenta to support the growth of the developing fetus. However, there is still a great deal to learn about the signals that regulate polyploidization and the specific function that polyploid cell types play in our bodies.
The only potential danger would be if a polyploidy cell somehow gained the ability to divide, which could pose a risk of aneuploidy, in which errors in the number of chromosomes per cell occur as a result of cell division. In the rare instances in which polyploid cells gain a mutation or an oncogene is expressed there could be a risk of developing tumors. Yet, cancer is rare in heart and muscle tissues, both of which are made up of polyploid cell types. The risk posed by polyploidy to human health therefore depends on the type of tissue and the conditions.
I didn’t know so many tissues have polyploid cells!
Usually scientists don’t realize it unless it’s something they’re looking for. It’s an area of biology we still need to understand more about. Most of what we know about polyploidy comes from research in plants and insects, where it is very common. In mice and humans, we still think of polyploid cells as being very specialized, such as the megakaryocytes in the blood or the giant trophoblasts in the placenta. But based on my findings, polyploidy appears to be more common than previously thought. We now need to understand its role in tissue development and function, as well as in tissue repair.
Do we know how the body decides which mechanism is used, cell enlargement or proliferation? Or can both take place together?
These are the major questions my group is interested in answering. There are examples in which just one takes place and examples in which both do. The liver is one of the most regenerative organs in the body — you can surgically remove 70% of it and it will regenerate and reform to its normal size. This occurs through both the division and the growth of hepatocytes. Researchers using a liver injury model in the mouse have found that if you inhibit cell division, the liver can still fully regenerate through the polyploid-dependent growth of hepatocytes. The regenerated liver still reaches normal size despite being composed of fewer, yet bigger, cells, which remarkably appear to function normally. Likewise, if you inhibit the ability of the hepatocytes to grow by polyploidization, the liver can still fully regenerate through cell division. This may be one of the reasons why the liver is the most regenerative organ in our bodies: it utilizes these two strategies simultaneously to repair and regenerate.
We don’t really understand why cells will heal a wound or repair a tissue by growing in some cases and by dividing in others. My goal is to understand how that decision is made by taking advantage of tools and software to dissect the genetic pathways and the molecular mechanisms involved.
You identified WIP by looking at Drosophila and, along with others, have demonstrated that the process occurs within mammalian organs such as the liver, heart and cornea. Do you think this is potentially a common mechanism for all tissues that could translate to other body parts, or just epithelial tissues?
I found that WIP occurs in mammalian corneal endothelial cells, while other researchers have found that a similar repair process occurs in the liver. I do think this is a general mechanism that is not specific to one tissue or another — one that could be used in any tissue type or organ in our bodies. My current hypothesis is that the determination of whether a cell will divide or grow to heal a wound is made by a combination of the signals a cell receives, as well as its intrinsic properties.
What are the steps to finding out if this wound healing mechanism could be boosted in humans?
The key to finding out if we can boost WIP in humans is to understand the molecular mechanisms that regulate it so that we can manipulate the response. We work with fruit flies because they are an excellent genetic model system: we can quickly dissect the genes and pathways that control growth. Fortunately, most of these genes/pathways are conserved in mammals, which will allow us to more easily apply our fruit fly research in a mouse injury model. If we find that the regulatory pathways have been conserved in the mouse, we will be poised to develop novel strategies to enhance tissue repair and wound healing in humans by boosting the WIP wound healing response.
For now, we still have a lot to learn about how WIP is regulated. We have identified several pathways that are critical in regulating this wound healing response, including the conserved Hippo and the JNK signaling pathways. Now we are trying to dissect how these pathways work in order to learn how to control the response. Interestingly, we have found that similar pathways regulate both mechanisms of tissue repair: proliferation and polyploidization. One of the things we are trying to understand is how similar genetic pathways can mediate two distinct mechanisms of tissue repair.
“I hope to see this knowledge translated to the clinic within my lifetime; we are at the tip of the iceberg at the moment. We’ve only recently discovered that polyploidy (cell growth) may be a beneficial part of the wound healing response rather than pathological one, as has been thought for so long. If we are to promote WIP as a means of tissue repair, we need to change the way we look at this response.”
What is a realistic timeline for developing a therapeutic approach for routine use in the clinic?
I hope to see this knowledge translated to the clinic within my lifetime; we are at the tip of the iceberg at the moment. We’ve only recently discovered that polyploidy (cell growth) may be a beneficial part of the wound healing response rather than pathological one, as has been thought for so long. If we are to promote WIP as a means of tissue repair, we need to change the way we look at this response.
Also, we still have a lot to learn about how polyploidy functions. We need to identify the key genes and mechanisms required to stimulate polyploidy and what distinguishes them from the mechanisms that control cell proliferation. I hope I will be able to apply what I’ve learned from the fruit fly to a mammalian model, such as the mouse heart or cornea within the next 5 years. We can then use targeted genetics to determine how polyploid-dependent cell growth affects the wound healing and repair response. If effective, this would be first step in developing a new wound healing therapy.

Do you have any initial thoughts on what form a potential therapy might take — for example a pharmacological agent or gene therapy?
Either is possible. People are already developing pharmacological agents and gene therapies that target the Hippo and JNK pathways because they are involved in tissue regeneration, cancer and many other things, so I think either has the potential to be used down the road.
What do you think is the biggest challenge in translating would healing research into clinical outcomes?
The biggest challenge is to more deeply understand how our organs initiate tissue repair when they are injured. Stem cells have been a remarkable discovery, in particular the fact that some tissues have resident stem cells that rejuvenate and protect our tissues against injury. And yet a number of our organs do not have stem cells. In organs without stem cells, researchers have attempted to transplant exogenous stem cells. So far, this approach has not succeeded, particularly in the heart. Stem cells rely on a microenvironment known as a ‘niche’ that supplies the external cues necessary to maintain their identity and function. Without an appropriate microenvironment, it’s hard to imagine how a stem cell could function normally and help regenerate damaged tissue.
As a result, we need to first understand how organs without stem cells normally repair themselves when injured. If we identify the self-healing mechanisms at play, then we can boost the organ’s innate ability to heal. This is where my research fits in. I think we need to start from the ground up and first understand how our organs go about healing when they don’t have a proliferative cell source. Once we understand these mechanisms, we’ll have a strategy to boost their healing capacity.
“In organs without stem cells, researchers have attempted to transplant exogenous stem cells. So far, this approach has not succeeded, particularly in the heart. Stem cells rely on a microenvironment known as a ‘niche’ that supplies the external cues necessary to maintain their identity and function. Without an appropriate microenvironment, it’s hard to imagine how a stem cell could function normally and help regenerate damaged tissue.”
What is the biggest challenge that you face in your research into wound healing?
I want to take what we have learned about wound healing from our fruit fly model and apply it to a mammalian model, such as a cornea endothelial injury model. Then we can test whether polyploidization is required for tissue repair and whether boosting endothelial cell growth through polyploidization can improve the cornea’s capacity for repair.
What else do you hope to achieve in the next 5—10 years of your career?
I would like to show that polyploid-dependent cell growth is a beneficial part of the normal wound healing response by seeing if it can improve tissue repair in many different mammalian tissues. In addition, it will be critical to determine if polyploid cells function similarly or differently than their diploid counterparts. We hope our findings will provide an alternative to stem cells transplants for wound healing and tissue repair. If our approach is successful, we will be poised to develop novel therapeutic strategies to promote polyploid-dependent growth and improve human wound repair.
Finally, if you had unlimited resources to carry our any work, what would it be?
As I mentioned earlier, we still don’t know how common polyploidy is within the human body. I would like to survey all human tissues to determine how many polyploid cell types are found in normal tissues and how many are found in diseased, injured or aged tissues. By identifying polyploid cell types we will not only be able to understand how common these cells are, but the unique functions they play in our bodies. In most cases, polyploid cells lack the capacity to divide. For example, heart cardiomyocytes, which are polyploid (tetraploid), only rarely divide. I found that corneal endothelial cells are polyploid. They too only rarely divide. For cells that don’t divide, polyploid-dependent cell growth offers an alternative strategy to regrow lost or damaged tissues. If we can identify the polyploid cell types in our bodies, we can target the appropriate cell types to stimulate WIP.
“I would like to show that polyploid-dependent cell growth is a beneficial part of the normal wound healing response by seeing if it can improve tissue repair in many different mammalian tissues.”
Executive summary
Further reading
- Losick VP, Jun AS, Spradling AC. Wound-induced polyploidization: regulation by hippo and jnk signalling and conservation in mammals. PLoS ONE doi:10.1371/journal.pone.0151251 (2016) (Epub ahead of print).
- Losick VP. Wound-induced polyploidy is required for tissue repair. Adv. Wound Care 5(6), 271—278 (2016).
- https://mdibl.org/press-release/new-mechanism-for-wound-healing-identified-by-mdi-biological-laboratory-scientist/