Extinguishing inflammatory bowel disease with enzyme inhibitors
Adverse symptoms of inflammatory bowel disease (IBD) in preclinical have been reversed using an enzyme-inhibiting drug.
DPCA, an enzyme inhibitor, has demonstrated promising outcomes in mitigating weight loss and repairing intestinal lining damage in mouse models of IBD, as highlighted in a recent study [1]. The research team, from the University of California, Berkeley (CA, USA), believes this approach could one day be used in conjunction with current treatment options or on its own to tackle the condition.
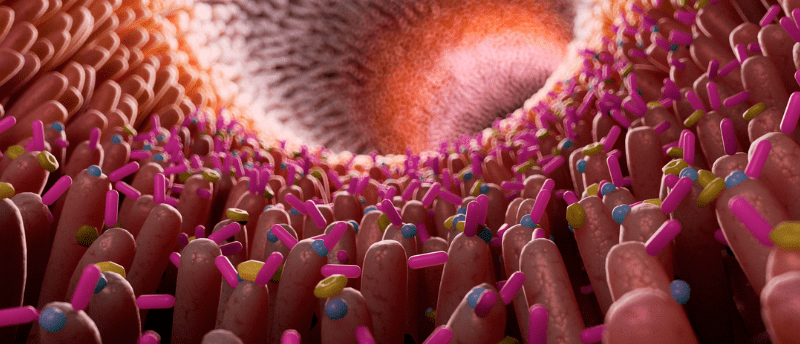
IBD is a chronic condition characterized by inflammation and ulcer formation in the colon and rectum, which is largely addressed with symptom-managing corticosteroids and biologics. While effective in providing relief from pain and inflammation, they do so without repairing the damaged intestinal lining.
In order to address this shortfall in the current standard of care, the research team set out to investigate the regenerative potential of an enzyme inhibitor called DPCA, which they have previously shown to have a regenerative effect on damaged or diseased tissues [2,3].
DPCA targets the HIF-1α pathway, which has been shown to play a supportive role in the regeneration of damaged tissues, and likely causes tissue regeneration through inhibition of HIF-1α-degrading enzymes. This enables migration of HIF-1α into the nucleus where it causes the upregulation of genes involved in cellular migration, metabolism and survival.
Using mouse models of ulcerative colitis, induced by exposure to dextran sodium sulfate (DSS), the authors investigated the effect of DPCA. The therapeutic molecule was embedded in a supramolecular hydrogel and delivered via subcutaneous injection.
In the first stage of the study, investigators tested the effect of pre-treatment with DPCA prior to disease induction. They did so by administering DPCA 2 days before the experimental condition: 10 days in a cage with drinking water containing 1.5% DSS, followed by 2 days of normal water. Mice that were pre-treated with DPCA before colitis induction did not develop intestinal lesions and had significantly less weight loss than controls.
The second experiment also saw mice exposed to drinking water with 1.5% DSS for 10 days, followed by a further 2 days of recovery with normal water. In this experiment, DPCA was administered on day 5. Compared to controls, there were several restorative effects, including accelerated weight recovery and epithelial lining repair as well as reduced expression of pro-inflammatory cytokines.
The researchers conducted further experiments to find out how epithelial cell lining regeneration was facilitated. They exposed colonic epithelial cells to DPCA and witnessed morphological changes indicative of an epithelial-mesenchymal transition. The researchers note that this dedifferentiation is an integral part of several species’ regeneration strategies, like axolotl.
“Based on our results, we think that short-term administration of DPCA may someday serve as a restorative therapy for IBD,” said Messersmith. “Ultimately, we want to find a way to turn back the clock for IBD patients and regenerate that [damaged] tissue back to the native tissue.”
This study demonstrates the potential of using DPCA for the therapeutic alleviation of IBD and represents a step towards harnessing curative treatments rather than therapeutics that manage its symptoms. However, there is still a need to map out the full effects of targeting the HIF-1α pathway, which possesses over 100 biological targets, before clinical stages are pursued.
You may also like:
 Could discarded neonatal stem cells treat Crohn’s disease?
Could discarded neonatal stem cells treat Crohn’s disease?
Heart-derived neonatal mesenchymal stem cells have been shown to reduce inflammation and promote healing in an animal model of Crohn’s disease.