Makin sense: 3D printing for preoperative consultations and consent

This column is the first installment of a series investigating 3D printing for surgical procedures, from preoperative consent to recovery.
Before any planned procedure, surgeons are required to gain fully informed consent from the patient. Guidance from the Royal College of Surgeons (London, UK), for example, states that a surgeon must:
‘Recognize that seeking consent for surgical intervention is not merely the signing of a form. It is the process of providing the information that enables the patient to make a decision to undergo a specific treatment. Consent should be considered informed decision making, or informed request. It requires time, patience and clarity of explanation.’ [1]
Whilst this may only be one point from a list of requirements covered by guidance relevant to ‘Good Surgical Practice’ and from only one body, this first point highlights key areas for where 3D printed, personalized models may aid surgical teams in achieving fully informed consent and confidence in their patient’s understanding of their condition, as well as the consultant’s treatment plan.
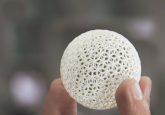
The collection of 3D data from patients has long been possible through MRI and CT scanning technologies, among others. Once the images have been segmented, DICOM data can be used to print replica models in a range of materials which may be able to match weight, color and even consistency of internal structures, enabling the physical presentation of a patient’s ailment in 3D as opposed to the examination of 2D images on a computer screen. Landmark structures such as the ribcage or replica organs can also be printed and incorporated into the model, informing the position of tumors or growths, for example, as well as reflecting relative sizes.
The physical handling of personalized models may incite more opportunities for patients to ask questions and better comprehend answers from their surgeons or consultants. A team of researchers from Seoul (South Korea) investigating the use of 3D printed personalized models with Stage I lung cancer found that models improved patient comprehension in informed consent for surgical resection of lung cancer tumors [2]. Patient knowledge was ranked significantly higher in questionnaires following consent consultations in a group exposed to half-life-sized models compared to groups without, leading the team to believe that the models improved patient understanding and therefore informed consent ahead of surgical procedures for this condition.
Similarly, Romanian scientists exploring malpractice and post-operative complaints found that 3D printed, personalized models worked in physicians favor when communicating the details of an ailment, the treatment options available and the possible outcomes. Complaints and patient dissatisfaction were reduced as a result of including 3D printed models in preoperative consultations [3], further making the case for 3D printing patient models ahead of surgical intervention.
From my own experience, I recently had the pleasure of interviewing Shana Cook (Milwaukee School of Engineering; WI, USA) for a 3DMedNet podcast investigating the use of 3D printing to improve patient experience. Cook explained the feeling of comfort and closure she experienced after 3D printing her tumor from her own MRI data and how being able to touch and feel a model of her tumor helped bring her condition to life, rather than struggle to understand the information previously presented to her in 2D on a computer screen.
“It’s hard to describe the feeling of holding the tumor model after it was printed. The physical model brought my understanding to a new dimension just like I brought the 2D images to a new dimension. I KNEW I had conquered this cancer, inside and out.” — Shana Cook for 3DMedNet

As a biomedical engineer with aspirations in the medical field, Cook is likely to have benefitted from a previous understanding of similar conditions and perhaps even a little experience of reading information from 2D and 3D diagnostic imaging. In complex cases involving children, the elderly or those who may struggle to provide fully informed consent, this may not be the case.
Certainly for complex cases, personalized 3D printed models could prove instrumental to developing an advanced and inclusive patient education model satisfying international consent guidelines, surgical teams and patients alike.
References
[1] Royal College of Surgeons: 3.5.1 Consent
[2] Yoon SH, Park S, Kang CH, Park IK, Goo JM, Kim YT. Personalized 3D printed model for informed consent for Stage I lung cancer: a randomized pilot trial. Semin Thorac Cardiovasc Surg. 31(2) 316—318 (2018)
[3] Tevanov I, Liciu E, Chirila MO, Dusca A, Ulici. The use of 3D printing in improving patient-doctor relationship and malpractice prevention. Rom J Leg Med. (25) 279—282 (2017)