Type-1 diabetes: substituting a lifetime of symptom management for interventive treatment
Lindsay Davies, Chief Scientific Officer, NextCell Pharma
 Lindsay Davies is the Chief Scientific Officer of NextCell Pharma (Huddinge, Sweden), a biopharmaceutical company that develops mesenchymal stromal cell products for autoimmune and inflammatory diseases. At this year’s Advanced Therapies Europe (ATE; 5-7 September 2023; Estoril, Portugal) we caught up with Lindsay to discuss the use of umbilical cord mesenchymal stromal cells in the treatment of type-1 diabetes, and the field-wide changes required to expand patient access to cell and gene therapies.
Lindsay Davies is the Chief Scientific Officer of NextCell Pharma (Huddinge, Sweden), a biopharmaceutical company that develops mesenchymal stromal cell products for autoimmune and inflammatory diseases. At this year’s Advanced Therapies Europe (ATE; 5-7 September 2023; Estoril, Portugal) we caught up with Lindsay to discuss the use of umbilical cord mesenchymal stromal cells in the treatment of type-1 diabetes, and the field-wide changes required to expand patient access to cell and gene therapies.
What are some of the current limitations in the standard of care for type-1 diabetes?
With type-1 diabetes, at the moment, the standard of care is symptom management and disease management. There are very few options for interventive therapies for the treatment of type-1 diabetes.
How can mesenchymal stromal cells be used to address some of these limitations?
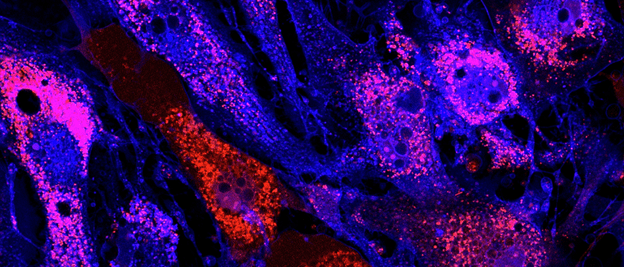
Our data using umbilical-cord mesenchymal stromal cells has demonstrated that the cells can interact with the patient’s own immune response, and they can sense the environment they’re put into. So, it’s a bespoke treatment for the patient themself. The umbilical cord mesenchymal stromal cells are also able to dampen destructive autoimmune responses and therefore prolong the patient´s own endogenous insulin production.
How are you currently working to develop this into a novel therapeutic for type-1 diabetes?
We are taking umbilical cord mesenchymal stromal cells from the tissue of the cord and expanding them in culture to generate therapeutic doses of drug product. We have a patented selection algorithm that allows us to select the best donor cells based on their ability to modulate immune responses. Once selected, we pool these donor cells together so that we can make larger batch sizes and reduce the batch-to-batch variability between our products.
These cells can be used as an off-the-shelf product, so we keep them in the freezer cryopreserved, where they can be shipped directly to the clinic. We treat using a fixed dosage, which means that there are no post processing-steps and there is no need to modulate the dose based on the patient’s body weight. This all allows us a much easier approach to commercialization.
These cells constitute a single treatment, given to the patient by peripheral infusion over 40 minutes. There are also no serious adverse effects associated with this treatment, meaning that the patient can be in and out of the clinic within an hour.
Is the therapy currently in clinical trials?
We’ve just completed phase II clinical trials in adults with newly diagnosed type-1 diabetes. The trials show the maintenance of endogenous insulin production during first year follow up, meaning that those patients that received treatment did not need to increase their insulin requirements throughout that whole year.
Having just passed the 3 year follow up, we still see a significant therapeutic effect for patients. We will continue to monitor these treated patients for a total of five years for safety and therapeutic efficacy. We have also just completed a Phase I pediatric safety trial and are entering into a Phase II pediatric trial as we speak.
Could this therapy be curative?
Our hope is that patients with type-1 diabetes treated with our umbilical cord mesenchymal stromal cell product will have delayed disease progression, lower exogenous insulin requirements, improved quality of life and fewer complications associated with the progression of type-1 diabetes.
If there was one you could ask for to optimize the use of this therapy, what would it be?
We need to invest in our patient populations. We have an aging population and events like the COVID-19 pandemic have taught us that we need to quicken our development processes whilst maintaining patient safety. At the same time, we need to invest in and embrace novel cell and gene therapies, because they offer potential treatments for diseases that lack treatment options. Financial implications shouldn’t be the reason that patients don’t have access to treatment.