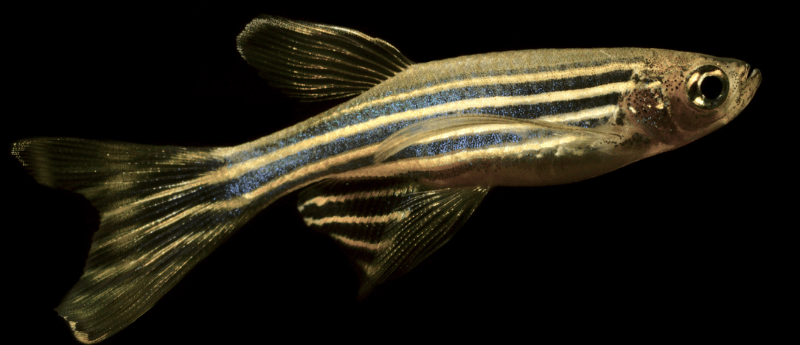
Can zebrafish proteins unlock the brain’s regenerative capabilities?
Two proteins found in zebrafish have been identified to counteract scar formation in the brain, thus improving the regenerative capabilities of the tissue.
A research team led by cell biologist Jovica Ninkovic from Ludwig-Maximilians-Universität München (LMU; Munich, Germany) has exhibited in Nature Neuroscience that lowering the reactivity of microglia is critical for the prevention of chronic inflammations and tissue scars and therefore enhancing regeneration potential.
Although cells in most endogenous tissues renew themselves on a regular basis, the amount of nerve cells in the human brain and spinal cord remains at a consistent quantity. However, LMU scientist Magdalena Götz has previously displayed that, outside of two specific areas of the brain, young neurons in patients with brain injuries are unable to integrate into existing neural networks and survive. This appears to be associated to glial cells, which create the brain’s supporting tissue. Microglia in particular can cause inflammation and scarring, which segregate the site of injury from the healthy areas of the brain. However, in the long term, microglia seem to inhibit the effective assimilation of new neurons into the neuronal system.
In contrast to humans, the zebrafish’s central nervous system (CNS) possesses excellent regenerative abilities. In the event of an injury, neural stem cells produce long-lived neurons. Additionally, CNS injuries cause only transient reactivity of glial cells in zebrafish, allowing nerve cells to integrate into wounded tissue locations.
“The idea was to tease out the differences between zebrafish and mammals so as to understand which signaling pathways in the human brain inhibit regeneration — and how we might be able to intervene,” explains Ninkovic.
During their experiment, the researchers caused CNS lesions in zebrafish to elicit the activation of microglia. They then discovered an accumulation of lipid droplets and axonal TDP-43 in the lesions. TDP-43 is a protein with implications in neurodegenerative diseases. The protein granulin was also found to play a significant role in the zebrafish model. Granulin aids in the elimination of the lipid droplets and TDP-43 condensates, at the point where the microglia switch from their active to their inactive form.
The result was the healing of the injury without any form of scarring. In contrast, zebrafish with artificially generated granulin deficiency showed poor healing of the injury, comparable to what we normally find in humans. “We suspect therefore that granulin plays an important role in the regeneration of nerves in zebrafish,” explains Ninkovic.
Ninkovic’s team also studied samples from people who had died from brain injuries to further examine the similarities between humans and zebrafish. Again, a direct correlation was found among the levels of microglia activation and the accumulation of lipid droplets and TDP-43 condensates. The results therefore displayed that parallel signaling pathways in human tissue were analogous with the same pathways in zebrafish.
The results of this study could inform future research into therapeutics for people with brain injuries. The research team at LMU intends to study if known low-molecular-weight drugs are suitable for suppressing signaling pathways of microglia activation, in turn enhancing the regenerative processes of neural legions.