Development of a liver patch for clinical use

In this community post, Matt Colender discusses development of a novel therapy to bridge the organ wait list gap.
A mouse runs around in the cage; then stops to clean her white fur. She puts her pink nose up and sniffs the air. Her whiskers wiggle.
US statistics have identified there are 120,000 patients a year waiting for organ transplant in the US alone; this number is much higher worldwide. Of those 120,000, only approximately 20,000 have transplants performed. 100,000 wait patiently for the call.
The mouse runs to the wheel, her pink feet start to turn it and she hustles.
One subset of these 120,000 patients is a group of about 11,000 pediatric patients with a handful of disorders of the liver that they were born with called inborn errors of metabolism (IEM). Examples of IEM include patients with fumarylacetoacetate hydrolase (FAH), ornithine transcarbamylase (OTC) and Alpha-1 antitrypsin deficiencies. These deficiencies are hereditary, passed down from a faulty gene in each parent that pair; creating a disorder in which abnormal chemical reactions occur in the child. Treatments for metabolic liver disease may include dietary changes, phlebotomy, medications and phototherapy, but most eventually require a liver transplant; usually in adolescence.
However, only a fraction of the patients who need these transplants ever receive them. Unfortunately, some that receive them reject them.
The mouse finishes her workout and sees that lunch has been served. She grabs a pellet in both hands and looks out inquisitively, and chews. Why is this mouse special? She was born with a liver IEM. Her liver function and IEM have been improved through implantation of a 3D printed patch!
An amazing bit of science is taking place in San Diego. A company named Organovo (CA, USA) is working on a solution for these pediatric patients.
Preclinical data continues to show increased durability of the liver tissue and strong early evidence of successfully impacting the disease state in animal models
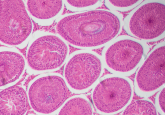
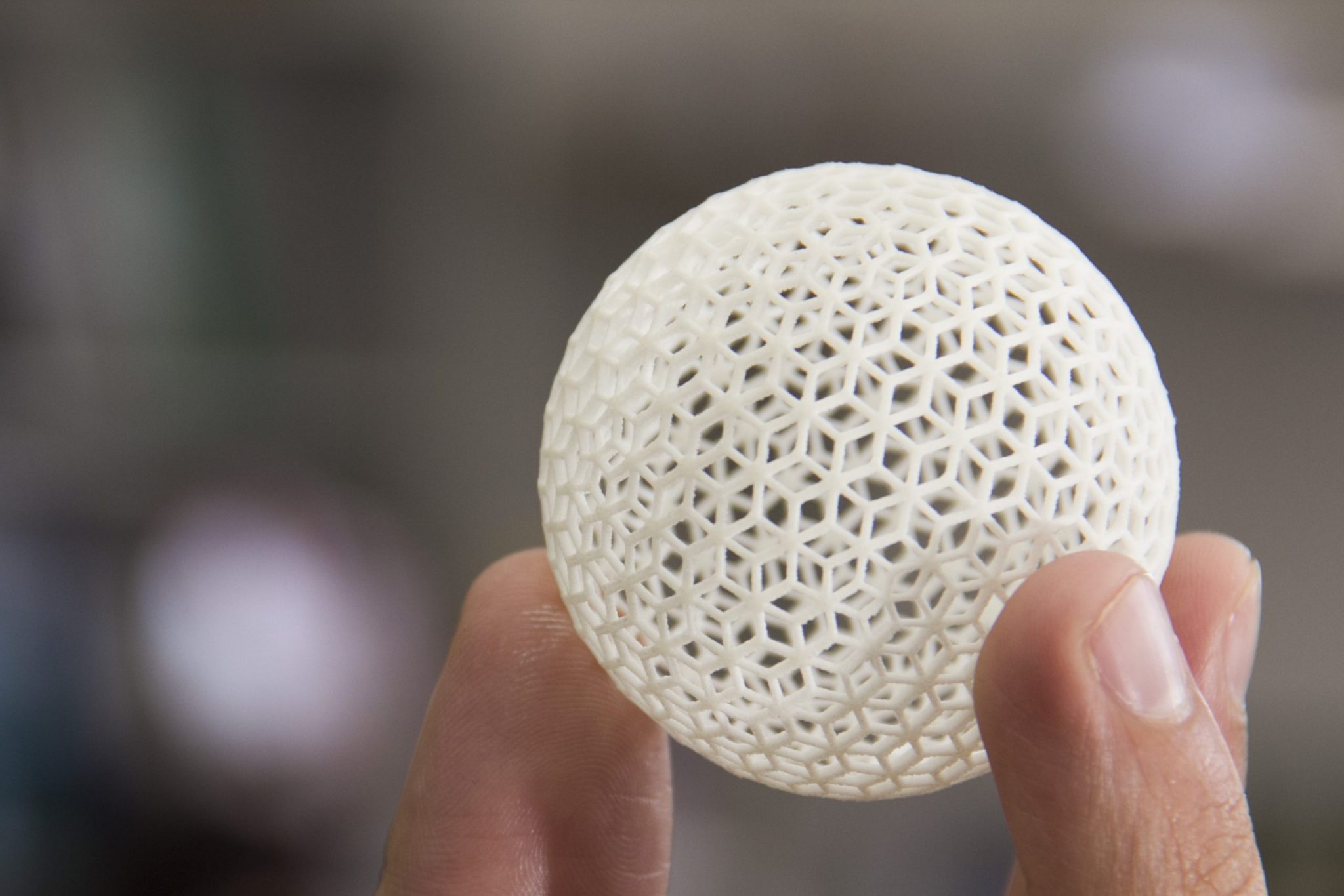
The Organovo team designed this mouse liver patch at the headquarters in San Diego. The first step was to develop the bioprocess protocols required to generate the multi-cellular building blocks–also called bio-ink–from the cells that would be used to build the target tissue. In this case, for the liver, they used human hepatocytes and select non-parenchymal cells (hepatic stellate cells, endothelial cells and kupffer cells). The bio-ink building blocks were then dispensed from the Novogen MMX bioprinter, using a layer-by-layer approach that was scaled for the mouse liver patch. The cells; at the right temperature and in the approximately correct architecture; accepted their surroundings and grew to form the tissue for the patch. They became viable living tissue.
Organovo have bioprinted liver tissue in this manner and implanted it into several NOD/SCID (impaired T and B cell lymphocyte development and deficient NK cell function) mice as a patch for the liver to show metabolism function improvement. The findings were presented at the Tissue Engineering and Regenerative Medicine International Society (TERMIS) annual conference in 2017. The results were astounding.
“Our preclinical data continues to show increased durability of the liver tissue and strong early evidence of successfully impacting the disease state in animal models,” Eric David, chief of strategy officer and executive vice president of preclinical development at Organovo, said in a statement.
“The robust presence of key human metabolic enzymes, which we previously disclosed, is also a critical step in demonstrating the capability of this tissue to treat IEMs, a key indication we are targeting. Taken together, these data supported continued preclinical development of Organovo’s 3D bioprinted liver tissue for therapeutic use.”
They demonstrated that the liver “patches” engrafted and perfused and that the blood serum detected human liver specific proteins and enzymes. In addition to showing the metabolic benefit of the specific patch area; the tissue around the patch began to heal, suggesting a potential curative effect.
Organovo believes that a dollar bill or cell phone-sized patch of 0.5–1mm thick bioprinted tissue could be a bridge for a patient waiting for transplant; a band aid, of sorts, that would carry a patient to a successful transplant who may not ever have had the opportunity before.
The company is currently mid-preclinical stage. At their lab in San Diego, they have mice with the bioprinted tissue patches running around now, which are being studied and have been shown to be functional past 90 days on their way to 120 days and beyond.
Read more about Organovo on 3DMedNet:
Organovo also contracts with pharmaceutical companies like Merck (NJ, USA), Roche (Basel, Switzerland), Bristol Meyers Squibb (UK), Astellas (Tokyo, Japan) and many others around the globe to test drug compounds on their bioprinted liver and kidney tissue to look for toxicity signals. The bioprinted tissue has been far more predictive of potential toxicity than the old methods which are still in use. The “old” liver toxicity protocol model, still widely being used by the FDA as the Gold Standard, is human liver cells, 2D in a petrie dish that do not survive past 48 hours and giving a weak toxicity testing gateway for drugs to pass FDA standards.
There are many notable drugs that passed this threshold only to make it to Phase III and have toxicity failures that cause them to be pulled. In addition, the method listed above is for liver toxicity. There is no method for kidney toxicity testing and Organovo can help in that aspect, as well with the bioprinted kidney tissue. They are also working with the Knight Cancer Institute (OR, USA), the Michael J Fox Foundation (NY, USA) and the Methuselah Foundation (VA, USA) for breakthroughs in disease and longevity.
The world is changing, as well. The 21st Century Cures Act calls for streamlined adoption of tissue and cell-based therapies. As described in Section 3033 of the 21st Century Cures Act, a drug is eligible for regenerative medicine advanced therapy (RMAT) designation if:
- The drug is a regenerative medicine therapy, which is defined as a cell therapy, therapeutic tissue engineering product, human cell and tissue product, or any combination product using such therapies or products, except for those regulated solely under Section 361 of the Public Health Service Act and part 1271 of Title 21, Code of Federal Regulations;
- The drug is intended to treat, modify, reverse, or cure a serious or life-threatening disease or condition; and
- Preliminary clinical evidence indicates that the drug has the potential to address unmet medical needs for such disease or condition
The robust presence of key human metabolic enzymes…is a critical step in demonstrating the capability of this tissue to treat IEMs
The FDA will be looking at bioprinting and all the benefits it provides.
The mouse stands up on her hind legs and rests her arms on the glass, and peers out over the scientists. She sees them out there in the lab, working hard for a better way. The tissue is working and there is a bright hope for the future. The mouse stretches and heads back for a nap, dreaming of a wonderful future.