First functioning human muscle grown from iPSCs
Engineers at Duke University have demonstrated for the first time that functional human muscle can be grown from non-muscle cells.
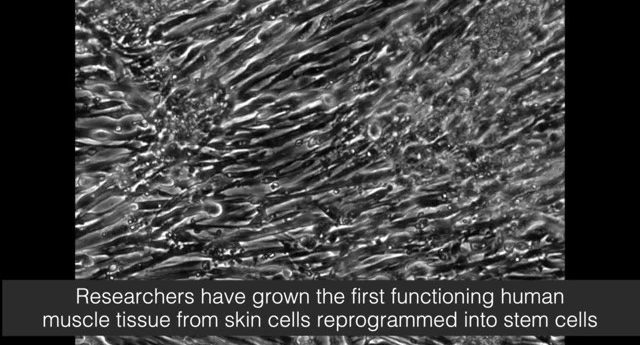
For the first time, biomedical engineers led by Nenad Bursac, professor of biomedical engineering at Duke University (NC, USA) have demonstrated that induced pluripotent stem cells (iPSCs) from non-muscle cells can be utilized to grow functioning muscle tissue. The results were published in Nature Communications.
“Starting with pluripotent stem cells that are not muscle cells, but can become all existing cells in our body, allows us to grow an unlimited number of myogenic progenitor cells,” commented Bursac. “These progenitor cells resemble adult muscle stem cells called ‘satellite cells’ that can theoretically grow an entire muscle starting from a single cell.”
Building on previous work utilizing myoblasts, cells that were past being stem cells but hadn’t matured into mature muscle fibers, Bursac et al produced iPSCs from adult tissue such as skin or blood. They were then cultured whilst being flooded with Pax7, a protein that encourages the cells to become muscle.
After 2-4 weeks of 3D culture, the grown muscle cells forms fibers that responded to external stimuli such as electrical and biochemical signals, mimicking neuronal inputs. The muscle cells also survived and function for at least 3 weeks when implanted into adult mice, integrating into native tissues through vascularization.
Although the resultant muscle was not as strong as native muscle tissue, falling short of muscle grown from biopsies, it still holds great potential. The iPSC-derived tissue developed much larger reservoirs of satellite-like cells that can repair damage, compared to the biopsy-derived tissue, and can also produce more muscle cells from less starting material. This technique could hold promise as therapy for genetic disorders. Genetic malfunctions could potentially be fixed in the iPSCs and the subsequent tissue used to heal localized problems. The technique will now be refined to grow more robust muscle.
“The prospect of studying rare diseases is especially exciting for us,” explained Bursac. “When a child’s muscles are already withering away from something like Duchenne muscular dystrophy, it would not be ethical to take muscle samples from them and do further damage.
“But with this technique, we can just take a small sample of non-muscle tissue, like skin or blood, revert the obtained cells to a pluripotent state, and eventually grow an endless amount of functioning muscle fibers to test.”
Sources: Rao L, Qian Y, Khodabukus A, Ribar T, Bursac N. Engineering Human Pluripotent Stem Cells Into a Functional Skeletal Muscle Tissue. Nat. Commun. 9, 126 (2018); https://www.eurekalert.org/pub_releases/2018-01/du-egf010518.php