Laboratory-grown red blood cells transfused into humans in a pioneering clinical trial
In the groundbreaking RESTORE clinical trial, laboratory-grown red blood cells (RBCs) have been transfused into patients for the first time, potentially opening the door to future therapies for blood diseases. The trial is being jointly led by research units from the University of Bristol (UK) and NHS Blood and Transplant (NHSBT; UK) to investigate the lifespan of RBCs manufactured from adult stem cells.
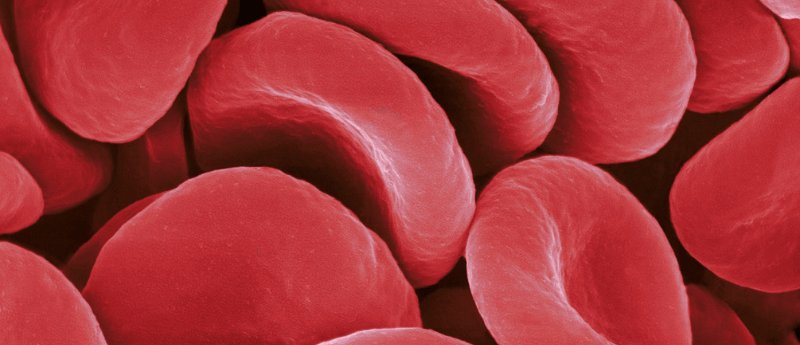
The RBCs were manufactured in the laboratory using stem cells acquired from donor blood. Magnetic beads were utilized to identify suitable stem cells with the ability to differentiate into RBCs. These cells were then placed in a nutritional solution which promoted proliferation and growth into mature cells over a period of around three weeks.
The cells were purified to remove other cell types before being preserved and later transfused into the patients. The lab-grown blood was labeled for the study with a radioactive substance to track how long it circulated in the body.
So far two patients have participated in the study, with no adverse side effects and this will be extended to a minimum of 10 volunteers who will receive two mini blood transfusions, one consisting of standard RBCs with varying ages and one of freshly manufactured lab RBCs. The lifespan of the cells from each infusion will be compared. The quantity of lab-grown blood cells being infused will vary between five to 10ml.
The team hypothesizes that the manufactured RBCs will last longer in the circulation of the volunteers compared to those from blood donors.
The researchers have emphasized that the aim of the trial is not to replace blood donations, the primary source for transfusions, but rather to assist patients with complex transfusion needs. A challenge faced by people with blood disorders such as sickle cell disease and rare blood types is finding well-matched donated blood. These manufactured blood cells could potentially revolutionize therapies for people affected by these diseases and, if proven safe and effective, provide a novel transfusion product for these patients. It is also hoped that this could minimize the frequency of transfusions for patients who frequently require blood transfusions and could help avoid iron overload, a severe complication linked with repeated blood transfusions.
“We hope our lab-grown [RBCs] will last longer than those that come from blood donors. If our trial, the first such in the world, is successful, it will mean that patients who currently require regular long-term blood transfusions will need fewer transfusions in future, helping transform their care,” says Chief Investigator Cedric Ghevaert, Professor in Transfusion Medicine and Consultant Haematologist the University of Cambridge (UK) and NHSBT.
The clinical trial is a significant step in making lab-grown RBCs a future clinical product and in improving the treatment for patients with blood disorders and rare blood types, although further trials will be needed before clinical use.
“It’s really fantastic that we are now able to grow enough [RBCs] to medical grade to allow this trial to commence, we are really looking forward to seeing the results and whether they perform better than standard [RBCs],” says Rebecca Cardigan, Head of Component Development at NHSBT and Affiliated Lecturer at the University of Cambridge.