Tissue-type plasminogen activator and human NPCs: two peas in one spinal cord
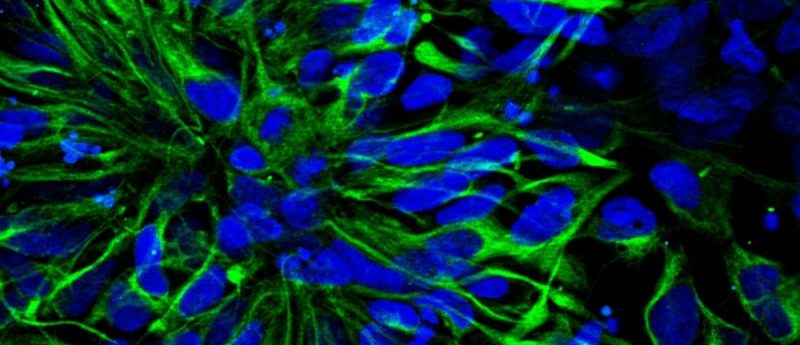
In this editorial, Pinar Mesci, Ph.D. (Assistant Project Scientist in Dr. Alysson Muotri’s laboratory, University of California San Diego) discusses her research on neural stem cell transplantations. Read Pinar's recent article, "Tissue-type plasminogen activator-primed human iPSC-derived neural progenitor cells promote motor recovery after severe spinal cord injury", here>> Stem cell therapy, initially limited to bone marrow transplants, has been a promising avenue in several fields of medicine, specifically in blood-related disorders. Since the first derivation of human embryonic stem cell (hESC) lines and the recent advances in induced pluripotent stem cell technology (or iPSC), we have now a unique opportunity...