Reducing stem cell variability with automation for standardized treatments: an interview with NYSCF’s Scott Noggle
In this interview, Scott Noggle, Senior Vice President of Research at the New York Stem Cell Foundation Research Institute discusses why he is fascinated by stem cells and why variability in their production has hampered efforts to find new treatments.
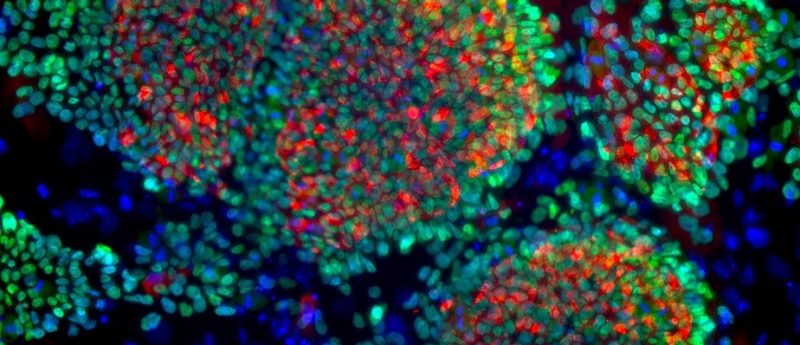
Banner image credit: Liheng Wang, The New York Stem Cell Foundation Research Institute
In this interview, Scott Noggle, Senior Vice President of Research at the New York Stem Cell Foundation (NYSCF) Research Institute, explains the important of standardizing methods of producing stem cells and the future for stem cell therapy.
Scott Noggle
Scott A. Noggle is the Senior Vice President for Research at the New York Stem Cell Foundation (NYSCF) Research Institute. He was a postdoctoral fellow at The Rockefeller University and he received his PhD in Molecular Medicine from the Medical College of Georgia. He has a long-standing interest in the derivation and use of human stem cells to understand human development and disease. Currently, his lab is applying new advances in pluripotent stem cell biology and cell reprogramming to the creation of human models of neurodegenerative diseases, such as Alzheimer’s disease and Parkinson’s disease to discover new disease targets. He also directs a group at NYSCF developing large-scale automated systems that use stem cells as a tool to understand how our genetics impacts susceptibility to these diseases. He and his team have developed high throughput automated systems for deriving new stem cell lines and differentiated cells to study disease models from large numbers of patients in parallel.
Can you introduce NYSCF?
I’ve been with the foundation for almost 9 years now. The foundation was started to accelerate the use of stem cells to find cures for different diseases that can be better understood by utilizing stem cells. The foundation has grown in the last 10 years and we’re now in our 12th year.
Our program covers three main areas: the first is an external granting body where we support postdoctoral fellows and young investigators from institutions around the world. This is a large program that we’ve built, with a community of over 100 scientists receiving grants. They are all at the top of their field in both stem cell biology and neuroscience, and have an interest in developing stem cells or neuroscience towards a translational goal.
Another aspect is the conference that we hold every year at Rockefeller University (NY, USA) which we think is one of the best on translational stem cell research that’s out there and it’s been an annual conference for the past 11 years. The final aspect is our research institute with the laboratories that we’ve been developing over the last 11 years. We started with the goal of enabling pluripotent stem cell (PSC) research under the difficult political restrictions of the time and over the past 10 years we’ve developed our capabilities around deriving and using stem cells as a tool to model disease. We’ve built a internal group of about 50 scientists that look at different aspects of PSC biology and its relevance towards various diseases such as Alzheimer’s, Parkinson’s, diabetes and multiple sclerosis. We also have bioengineering groups that look at topics such as developing bone tissue for potential grafting. Essentially, our aim is to become a bridge between the academic and the industrial worlds, and help these great discoveries in stem cell biology make their way into clinical applications.
What interests you about stem cells?
I think they’re fascinating! I got hooked on stem cells as a research topic in grad school. My PhD advisor, trying to attract grad students into the program, showed a video of mouse embryonic stem cells (ESCs) that had been differentiated into cardiomyocytes. They were sitting a dish beating with the rhythm of the heart and that really captured my imagination.
Over the past 15-20 years, I’ve been looking at how different tissues are built using embryonic cells. My interest has been in how the body builds tissues from pre-existing undifferentiated cells with a particular focus on building the nervous system. My PhD and postdoc work was focused on early neurodevelopment and how the early brain is specified. Here at NYSCF, I’ve continued to focus in on that area and tried to adapt what we’ve learned to try to model different neurodegenerative diseases like Alzheimer’s and Parkinson’s.
How did you become involved with the NYSCF?
I was recruited from Rockefeller, where I was running the stem cell derivation core facilities for the “tri-I” institutes here in New York — Rockefeller, Sloan-Kettering and Weill—Cornell (both NY, USA). I had been deriving ESCs and studying PSC biology and neurobiology at Rockefeller. The lab at NYSCF had been running for about a year and the foundation was looking to build up the internal research capabilities. I was recruited to help built a research program here within the foundation and the research institute.
Why have you chosen to focus on neurodegenerative disease as a target for stem cell therapeutics?
My interest in how the brain develops in the embryo led to a focus on creating the various types of cells that are affected by disease such as Alzheimer’s and Parkinson’s. With a personal family history of dementia, it’s always been an interest of mine to figure out how these diseases work. How does the brain first put together a tissue and how does this disease then destroy them? That’s the main focus of my interest in developing stem cells.
What are some challenges that you have faced in this research, for example when producing the PSC, and how did you overcome them?
When we started deriving the ESCs, it was very much an artisanal process. It was very laborious, with manual micromanipulation of cells to produce the cell lines, and everybody had developed their own special techniques and recipes for doing it. As a consequence, there were a lot of variations that weren’t disease specific in the qualities of the lines. We found that that variability had historically been present in the field due to a small number of people using a large number of different techniques to derive and develop the stem cell lines, and the ability to reproduce findings has been hampered by the technical variation. We’re still seeing efforts towards producing differentiated cells that could be used in various cell therapies and therapeutic applications being hindered by variable starting material. It can sometimes be one of the biggest bottlenecks in developing therapeutics.
The various media, processes and techniques that have been improved upon over the years have helped to standardize a lot of the methodologies. However, we have focused a lot of our efforts on finding ways to reduce the remaining variability and understand where the variability comes from. We’ve also tried to find standardized procedures, for example, utilizing automation, that allow us to methodically derive cells to reduce a lot of that technical variability. We’re really trying to uncover the inherent biological variability that might lead to differences in disease phenotypes, as well as responses to different drugs.
What prompted the development of the NYSCF Global Stem Cell Array?
Reducing the variability of the derived cell lines in the first place was a large component of it. We drew on our experience from the genomic world, in automating the various steps in doing genome analysis, as well as the pharmaceutical world, in doing drug screens. Over the past 5 years, we have developed liquid handling robotics and methodologies for standardizing cell culture.
However, the other component of it is the desire to be able to do the equivalent of genome-wide association studies in vitro and the ability to link in vitro phenotypes to genotypes in an effort to uncover new genetic pathways that are responsible for various diseases. Therefore, our initial goal in developing the NYSCF array was the ability to produce many stem cell lines from individuals in parallel, reducing variation whilst eliminating a lot of the technical variation to uncover disease relevant biological variation and genetic variation.
Why is integrating automation into laboratory workflow important?
The ability to automate and eliminate technical variations is critical in understanding the biological questions that you’re interested in, for example where there are quantitative genetic impacts on phenotype. Here at NYSCF, we’ve automated not just stem cell culture, but a lot of the assays that we use for analyzing the stem cells. We remove spurious technical variation which allows you to have more confidence in the underlying biological observations that you’re making.
I have found that even for biological questions that traditional academics would answer at the bench, automation and the capability to automate assays has really improved our ability to repeat our observations, as well as uncover signals that may previously have been swamped out by technical noise.
What obstacles are there to widespread adoption of automation in labs around the world?
A large obstacle is cost; these robotic systems can be quite costly to install in common laboratories or core facilities where I think they would be really valuable. There also needs to be a cultural shift to encourage biologists to work with the engineers that have the expertise to program and adapt biological assays to the automation. For instance, at NYSCF, we’ve assembled teams of biologists that work with engineers who can very quickly adapt protocols to automation. However, it does require concerted efforts to marry those two worlds of engineering and biology.
What is the future for stem cell therapy?
I’m quite optimistic! I think we are making good steady progress towards the development of cell therapies and using stem cells as a tool to understand the mechanisms of disease and find new drugs or therapeutics. In the long term, I think that cell therapy applications will be important. However, I think the ability to modify or prevent appearance of these diseases utilizing stem cells as a tool to find new therapeutics will be another valuable contribution that stem cells will make.
There are already drugs that are entering the early phases of clinical trials that have been developed using stem cells as an important tool in the development process. There are a number of cell therapy trials that have already started and that we’re anxious to see the initial results. Understanding how these diseases work on the cellular level utilizing stem cells will further our ideas of how to advance these therapies. I think that the future is quite bright; I think we’re well on our way towards the therapies that we’re really interested in developing in the long term.
Acknowledgements/Disclosure
- Scott Noggle is an employee of NYSCF.
Further reading
- Yaffe MP, Noggle SA, Solomon SL. Raising the standards of stem cell line quality. Nat Cell Biol. 18(3), 236-7 (2016)
- Paull D, Sevilla A, Zhou H. Automated, high-throughput derivation, characterization and differentiation of induced pluripotent stem cells. Nat Methods. 12(9), 885-92 (2015)