Surprising discovery in prostate gland regeneration study
A team at Memorial Sloan Kettering Cancer Center (NY, USA) have found that, instead of a smaller subset of cells driving regeneration, almost all remaining cells contributed to gland regrowth, in a murine model.
Researchers investigating prostate gland regeneration after treatment for advanced prostate cancer have demonstrated that nearly all cells present after treatment acquired stem-like properties.
Charles Sawyers and his team at the Memorial Sloan Kettering Cancer Center (NY, USA) expected a rare population of stem cells was responsible for regeneration; however, the study, recently published in the journal Science, determined that almost all cells present after therapy contributed to regeneration. This has important implications for how doctors treat prostate cancers.
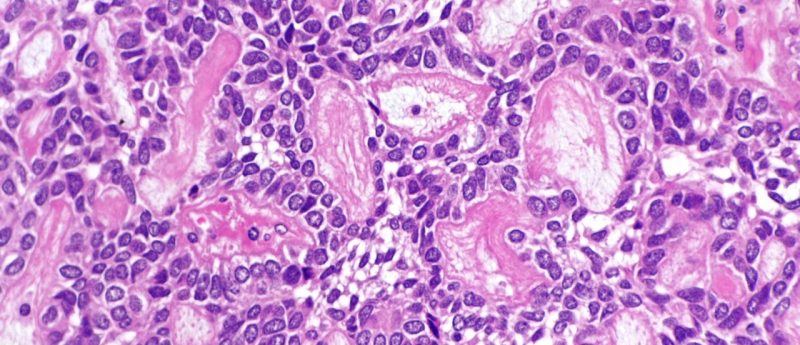
Androgen deprivation is the standard treatment for men with advanced prostate cancer, resulting in a 90% reduction in prostate gland size due to the loss of luminal cells. However, the cells that remain can eventually regrow and can often be resistant to further treatment, as well as increasingly likely to metastasize.
In collaboration with the Dana Pe’er lab in the Sloan Kettering Institute and Aviv Regev’s lab at the Broad Institute (MA, USA), the team used single-cell RNA analysis to sequence almost 14,000 cells in the mouse prostate gland. They could then determine which cell types were responsible for prostate gland regeneration post-therapy, discovering that luminal cells acquired abilities they don’t usually have in hormonally intact animals.
“They became much more stem-like,” said Wouter Karthaus, a senior postdoctoral fellow in Sawyers’ lab. “Without androgens influencing their gene expression, they were free to turn on other genes and acquire regenerative properties.”
Their regenerative ability was partly attributed to androgen-driven expression of growth factors Nrg2 and Rspo3 by mesenchymal cells acting in a paracrine fashion on luminal cells.
Moreover, analysis of human prostate tissue revealed similar stem-like behavior of luminal cell populations, suggesting that human prostate gland regeneration was comparable and driven by the majority of cells, not just by rare stem cells.
This study builds on earlier work from the Sawyers lab, where it was demonstrated that some prostate cancer cells have lineage plasticity. They established that they can become a type of prostate cell that does not require androgen to survive and therefore able to develop resistance to hormone-blocking therapies.
The findings of the new study could have significant implications on how doctors treat prostate cancer. “Androgen-deprivation therapy may be a double-edged sword,” Dr Sawyer commented, adding that “it is likely that we push prostate cancer to have a more progenitor-like state during therapy.”
Further work will investigate the molecular and cellular cues responsible for changing the cell behavior, with the hope being that the switching mechanism can be turned off.
Source: https://www.mskcc.org/blog/new-discovery-explains-how-prostate-gland-regenerates-itself