Professionalizing mesenchymal stem cells: an interview with Tony Ting
The regenerative medicine industry has transformed and diversified over the years. The cell and gene therapy (CGT) space is faced with several challenges as it grows, from failed clinical trials to difficulty in commercialization.
In this interview we talk to Tony Ting, Chief Scientific Officer at Bone Therapeutics (Gosselies, Belgium), a cell therapy company specializing in addressing unmet medical needs in the field of orthopedics and bone diseases. Tony discusses the evolution of the CGT space, the benefits of iPSC-derived mesenchymal stem cell (MSC) products and the future vision of Bone Therapeutics.
Could you please give us an introduction to yourself, your background and bone therapeutics?
I’m the Chief Scientific Officer for Bone Therapeutics. I joined in April 2021, during the pandemic, and prior to Bone, I’d spent 20 years at Athersys (OH, USA) where I was the Vice President of Regenerative Medicine and Head of the Cardiopulmonary programs. At Athersys, I worked from the bench to the bedside and was involved in all aspects in the development of MultiStem®. I ended up running a number of clinical trials including acute myocardial infarction, as well as acute respiratory distress syndrome (ARDS), which is now well known due to COVID.
I have been exposed to this space for quite a long time and I have seen the evolution of cell therapy grow dramatically. Within the past 5 years we have seen significant gains in the field, mainly due to the explosion in the immuno-oncology space. I joined Bone for two reasons: they had a product which was at late-stage clinical trials, but more importantly, Miguel Forte had a vision of developing a new and improved MSC platform. That is what really attracted me – I’ve seen too many MSC-based clinical trials fail and I wanted to see if there was a way to make a more successful clinical product.
Why do you think so many trials fail at phase I, phase II and phase III stages, when they have seen so much activity preclinically?
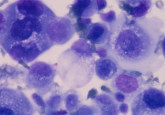
MSCs worked quite well in the animal models – there are thousands of papers with MSCs, with a fair few done on animals – and on ClinicalTrials.gov, there are over a thousand clinical trials conducted using MSCs, treating over 10,000 patients to date. Unfortunately, there are only a handful of approvals: one in Europe – darvadstrocel, an MSC-based product for direct injection into anal fistulas – and a few in Asia, including an approved product in Japan called TEMCELL® (JCR Pharmaceuticals; Ashiya, Japan), for the treatment of graft-versus-host disease (GvHD).
I think partly we have been asking too much of these cells. An issue that we face is heterogeneity: everyone has a slightly different version of MSCs. In many of the trials, researchers must use multiple MSC donors as they cannot get enough product from a single source. Therefore, there is heterogeneity of both the product and the patient population. Despite this, there is a slight gap where the cells do have benefit – they can secrete a variety of factors, modulate the immune system, dampen inflammation and promote angiogenesis – yet this is still not enough.
Bone Therapeutics has done two different things to address this issue. The first is a product called ALLOB, which is in Phase IIB clinical trials for difficult factors. ALLOB is an MSC-based product, but the cells are more osteogenic and osteoinductive, designed to accelerate bone healing.
Was expansion of volume and dose the driver for your agreement with Implant Therapeutics (MD, USA) to use iPSC-derived MSCs, rather than bone marrow?
No, that is for the next stage of evolution for our platform – we aim to focus on an iPSC-derived MSC product. By starting with an iPSC line, you avoid heterogeneity and only have a single source that can be well characterized. Cynata Therapeutics, a company based in Melbourne (Australia) is also doing this – they have conducted a phase I clinical trial for GvHD.
Bone wants to take advantage of the current robust iPSC technology and all the genetic engineering tools that are now available and have been approved by regulators. There is also an abundance of literature of genetic manipulations of bone marrow/adipose-derived MSCs demonstrating improved therapeutic benefit in animal models. Bone is pulling together all the existing knowledge to professionalize the MSCs.
We aim to genetically modify the MSCs. One method is to knock out the major histocompatibility complex class I and class II, making the cells more persistent, to prevent them from being quickly cleared by the body – there is evidence to suggest that this is effective. Another method is to tailor specific genes of interest towards a particular therapeutic indication. For example, if we wanted to treat an acute unmet medical need involving inflammation, we may choose a specific gene that has been overexpressed in MSCs and has been demonstrated to enhance their anti-inflammatory capabilities. We are developing a platform that can use genes that have been identified as being important, overexpress them in the iPSCs and then differentiate them to MSCs – this will hopefully result in a more potent MSC product that will achieve success in the clinic.
Are you expecting the platform to have the capability to be applied to different indications and smooth the regulatory pathway?
Exactly! Once we have our chemistry, manufacturing and controls locked down, it will only be a matter of swapping out the gene. If we are successful with an acute indication, we would then have the ability to go after chronic indications. As we plan to delete the major histocompatibility complex class I and class II, there is less concern for immune rejection and we would gain the ability to do repeat dosing. There are a lot of chronic indications that have been explored in the preclinical data out there, such as multiple sclerosis or Crohn’s disease. Beyond that, we can think about neurodegenerative diseases – there are a lot of applications that are not in the immuno-oncology space that are areas of high unmet medical needs. These are the areas that Bone wants to go after.
With high unmet medical needs and expanding patient populations, how will we approach the challenge of reducing costs?
There are benefits to starting with an iPSC to bring down the cost of goods. There are challenges with MSCs, such as sourcing and reducing variability. iPSCs are a useful single source that is well characterized – this reduces the cost of goods.
How has the pandemic affected the progress of these clinical stage investigational drugs?
Similar to most other clinical trials, COVID has had an impact. There is constraint at clinical sites as research staff are now allocated to treating COVID patients. Recruitment of patients has also slowed down: as we focus on treating patients with difficult fractures of high impact, during the pandemic, people were not out in situations where they would get these types of fractures. We are trying to work with hospital sites or clinical sites to make sure they have the resources available to be able to conduct studies, though this has been a struggle because hospital systems are overburdened.
Are you concerned that the additional comorbidities of ARDS and long COVID may affect patient populations even further?
I’m sure there will be an impact, but not for ALLOB. We are focused on difficult fractures rather than immuno-oncology. As we establish our platform, we want to ensure that we choose an indication where we can recruit patients quickly and efficiently. Patients will play a key part as we want to make sure that the first product we create is successful.
Bone also has a lot of good experience that we can leverage. We have a team experienced in MSC-based product development. We have familiarity with regulatory requirements to get a product into the clinic. Further, we are working internally to develop a process that is scalable in order to achieve success in the clinic and commercial viability. With all this experience to leverage, we will be expanding Bone beyond the orthopedic area.
How would you define a ‘professional cell’?
In our case, the professionalized cell is the iPSC-derived MSC product where we have done genetic manipulation to ensure that the product is fit for purpose. I like to use the term bespoke.
There is an abundant literature talking about the genes that have been overexpressed in MSCs and have demonstrated additional benefit on top of standard MSC products in animal models. This is where professionalization comes in. We will be conducting our own pre-clinical studies to demonstrate that our chosen gene can enhance the MSCs therapeutic benefit – there have been several Phase III clinical trials that have been close but didn’t make the primary endpoint. One could argue that they didn’t choose the right endpoint, but ultimately the cells just didn’t deliver; it is asking too much to expect one cell to do heart failure, GvHD and ARDS. We need to identify which genes are effective when expressed, and make them bespoke for identifying, or professionalizing, the MSCs.
Any advice for other developers?
It is all about understanding the biology – do you understand the biology of your cell and can you translate it? It’s difficult and there are lots of components that one needs to consider, and it’s important to think about commercial manufacturing. There is a lot of equipment in place for biologicals and it’s being retooled for cell therapy products. It was great to see a large scale cryofreezer at the Phacilitate event – the field is anticipating commercial success.
How has your definition of ‘regenerative medicine’ changed while you have been in this field, and do you think it’s still a relevant term to be using?
It has changed quite a lot. When I first started, we thought we would differentiate cells into cardiomyocytes to rebuild the heart. We now think of regenerative medicine as a way to accelerate the healing of the endogenous body’s regenerative capacity. I would say regenerative medicine has broadened and is now focused on interacting with the human body to stimulate healing.
Disclaimer
The opinions expressed in this interview are those of the interviewee and do not necessarily reflect the views of RegMedNet or Future Science Group.